In 2012, when I came back to Córdoba — after almost 11 years in the United States — to work at the Instituto Modelo de Cardiología Privado SRL (IMC), I suggested to the board that the hospital didn’t need another cardiologist. Instead, I offered to leverage the lean knowledge I had acquired in the U.S. through research and connections to help the organization identify and solve its most critical problems and improve patient outcomes.
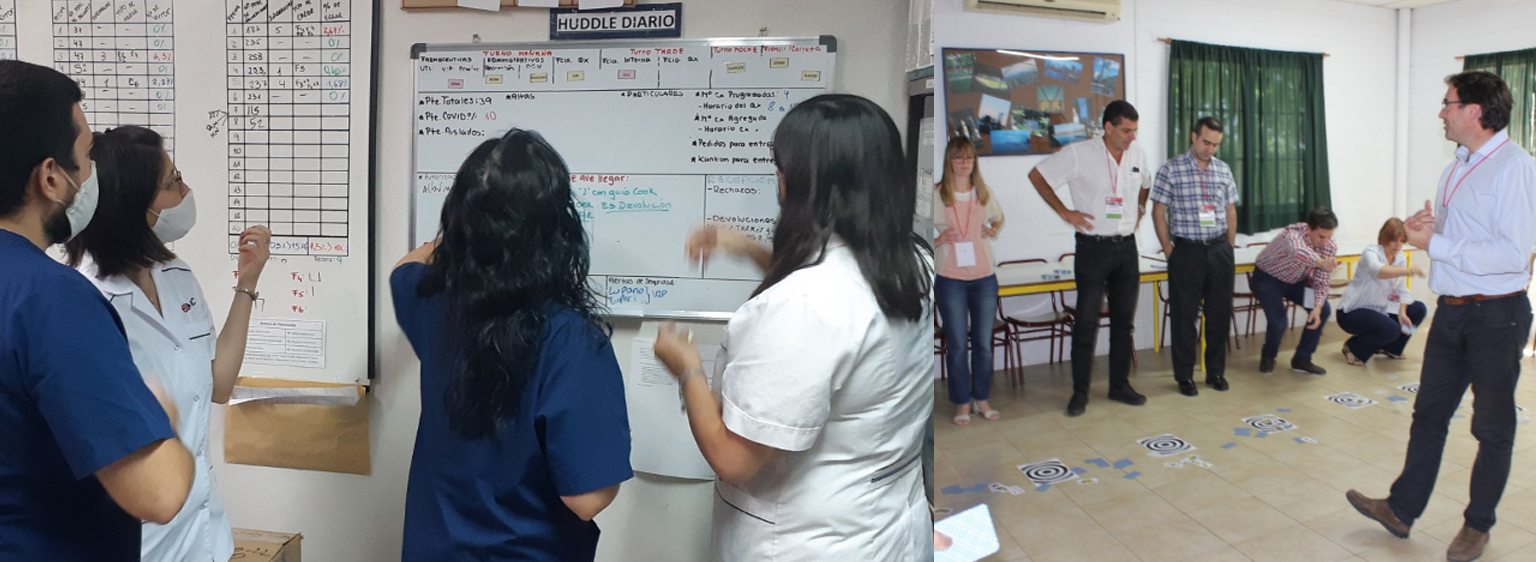
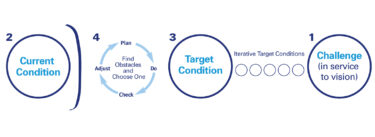
With the board’s full support and participation, one of the first steps was to reach out to the leaders of the various departments. We wanted to understand how they were managing their areas and what metrics they were using. What we found was that many of the department leaders had no clear idea of their current state. There were hardly any metrics being tracked and no visual management in place. There was a disconnect between these leaders and their teams and between the department and the organization’s True North. So, to bring visibility of the current state to the various hospital processes, we started measuring.

See the agenda and register for Lean Global Connection at https://planet-lean.com/lean-global-connection/
IMC is a 44-year-old “boutique” hospital. In 2019, we recorded 8,703 admissions and 238,000 outpatient visits (of which 57,284 were emergency visits). We only have 72 beds, but with more than 250 physicians, we provide 53 specialties. Cardiology is the main one. I knew that transforming a small but complex organization like ours would require patience, especially considering that not all physicians are always on-site (some are here for as little as two hours a week).
Getting everyone on board would be a challenge, which is why we began our improvement efforts in the areas and processes that seemed to respond most positively to the first timid lean steps we took. Three in particular — our cardiac rehabilitation program, laboratory, and pharmacy — became our model cells. We started to look into their processes, engaging local leadership and frontline staff in the improvement work.
Slowly but surely, the changes we made got the attention of other areas, and people started to get curious. In those first few years, our transformation efforts focused on the support functions rather than the physicians themselves — laboratory and pharmacy, of course, but also H.R., purchasing, and administration. We were hoping that improving these areas would capture the imagination of physicians and encourage them to get involved, too.
The first large-scale improvement directly led by physicians was in our operating rooms.
The first large-scale improvement directly led by physicians was in our operating rooms. In fact, it was them who asked for help. The problem was that surgeons often didn’t know when they were scheduled to operate because it was hard to understand when an OR was available and when it wasn’t. So a team was created — which included the Chiefs of Traumatology, Cardiovascular Surgery, Vascular Surgery, Operating Rooms, ICU, and Anesthesiology, as well as administrative staff, a board member, and myself — and a number of basic lean tools, like value stream mapping, were introduced to bring clarity to the situation.
Seeking Accreditations — and Excellence
We had desired that the hospital get more international accreditations. In 2016, we applied for the Chest Pain Center Accreditation Version 5 with Primary Percutaneous Coronary Intervention, then jointly awarded by the American College of Cardiology and the American Heart Association from the United States. It was a huge undertaking for us, but my hunch was that teaching our personnel how to apply lean thinking to our processes would help us get there.
Eager to deepen our understanding of lean, we managed to obtain a scholarship, sponsored by Cardinal Health (USA), to take a team to the States for two one-week training sessions at the Academy for Excellence in Healthcare at the Fisher School of Business at Ohio State University. They took place in July and October 2016, and we were the first international team (cohort 9) to participate in the program. The team consisted of the Chief of Heart Failure, the Chief of Post-Cardiovascular Surgical Care, the Chief of the OR, the Chief of the Cath Lab, and myself. To prepare and to get the team familiar with the lean lingo, we read together Management on the Mend by John Toussaint, as well as the program’s pre-reads.
Getting leaders from our hospital to visit other organizations that were further along in their journey opened their eyes to the opportunities afforded by lean.
In many ways, those two visits to the United States were a game-changer for the lean transformation of IMC. I had been frustrated with the slow progress and the physicians’ buy-in we had seen, and, as usual, the answer was in the gemba. Getting leaders from our hospital to visit other organizations that were further along in their journey opened their eyes to the opportunities afforded by lean. We’d visited the Ohio State University Wexner Medical Center in July (at the time, led by their Transformation Leader and Chief Quality Officer Susan Moffatt-Bruce, who was our coach during the training) and Cardinal Health’s main Distribution Center in October. That’s when things started to come together: on one hand, we had projects run by support functions across the hospital; on the other, physicians who were finally understanding the value of lean.
From 2012 to 2016, when our support areas drove the change, our progress was great but limited to the various silos and largely unseen by physicians. For example, even when we transformed the process in the operating rooms, they recognized it but still didn’t engage fully outside the O.R.s. Things changed after we went to the U.S., however. That’s when the physicians started to get involved, and we began to see more cross-functional projects and the systemic change they are capable of effecting.
As part of our training with the Academy, we completed a project to improve discharge time — a sticky point for hospitals around the world. By introducing flow to the process, we made great improvements. Between 2016 and 2017, we achieved our target of 40% of patients discharged before 10:30 AM, 60% before 12:30 PM, and 80% before 2:30 PM. (Today, in 2021, our target is 50%, 70%, and 80%, respectively.) Our work was documented in a White Paper.
Proving we were on the right track, in 2017, we received the much-wanted Chest Pain Center with Primary PCI accreditation. It took us less than a year. In 2018, we also got the ACC Heart Failure Accreditation — the only one outside the United States. Keen to build on our progress, we even brought the Academy to Argentina for three week-long teaching sessions and two week-long coaching sessions in 2018. Hosting the sessions represented another powerful catalyst for change, creating incredible synergies and awareness and greatly deepening our understanding of lean thinking.
Then we also won an ACC First Place award for quality improvement and received ACC recognition as an International Center of Excellence in 2019. The key to all these achievements was helping our people to speak the same language — that of lean thinking — and pulling forces to work toward a common goal. Ultimately, this has allowed us also to maintain our results over time.
I believe our approach … helped us get the leadership support we needed to drive transformation and identify our best change agents.
There is no doubt that another fundamental element in our transformation is the support we have received from leadership at all levels (without it, sustaining change is impossible, in my opinion). I believe our approach, which is based on continuously training leaders and educating from the top down, helped us get the leadership support we needed to drive the transformation and identify our best change agents.
When it comes to learning from others, we’ve had many lean experts visit our gemba, including Marcelo Zottolo, Susan Moffat-Bruce and Peter Ward from the US, Myrna Flores from Switzerland, and José Ferro and Frederico Pinto from Brazil. Some of them have given workshops, others have delivered lectures to share their vast knowledge. Going on gemba walks with them and receiving feedback on our A3s was fundamental.
With regards to sharing knowledge internally, word of mouth is still very much our modus operandi. It’s not structured, and it’s not what we want, but it works, at least until we can standardize and develop our own lean healthcare development programs (which we hope to accomplish this year). Through word of mouth, we have shared lean from one area to another within IMC — the same idea that is behind our Lean Day, an end-of-year get-together when people present their A3s.
We are also very proud to see how our lean efforts are inspiring other organizations. For example, after attending our Lean Healthcare Summit in 2018, the first ever in Argentina, we have seen many hospitals in Buenos Aires embark on their lean journeys.
Powering through the Pandemic
An article published in The Economist in October 2018 said that “most economies are ill-prepared for even a mild recession.” We could talk about “economies for hospitals,” and the sentence would still make perfect sense. In Argentina, we are sadly very used to economic turmoil: the country recorded an inflation increase of 53.8% in 2019 and 36.1% in 2020. In 2019 alone, our labor costs also increased by 53.8% and in 2020 by 21.4%. What do you do in a situation like this? Our response was clear: we need to create more value for patients. Like George Merck once said: “We try never to forget that medicine is for the people. It is not for the profits. The profits follow, and if we have remembered that, they have never failed to appear.”
Indeed, this idea has informed our improvement work since the very beginning, whether we were trying to answer our patients’ calls right away or improving the patient flow through ambulatory care. We have achieved great results by continually raising the bar, reminding ourselves that we can always do better and offer the patient a better experience. It’s worth remembering, for example, that while today over 90% of our patients go from reception to blood extraction in less than 10 minutes, our initial target was 15 minutes — in line with the 2016 Cleveland Clinic’s target.
Overall, since 2012 thanks to lean, the Instituto Modelo de Cardiología has achieved — before Covid-19 — increases of 31% for surgeries, 68% for admissions, 84% outpatient visits, 103% for E.R. visits (among other results). Lean thinking has allowed us to streamline processes, reduce waiting time for patients, and improve the quality of our care. Something I am very proud of is the fact that we were able to sustain these results throughout the pandemic, as well.
Over the past year, we had to pause many of our projects, as the fight against Covid-19 became our number one priority. This is a war, and we haven’t been strangers to loss (in fact, we lost some of our lifelong patients to this virus), but I think it’s also important to celebrate our successes: our in-hospital mortality for Covid patients is 10%, considerably lower than the global average, and in such complicated economic conditions here in Argentina we have been able to keep everyone on payroll.
I don’t know how we would cope with this emergency without lean.
It has been moving to see our staff come together and leverage their lean knowledge to protect each other and our patients as best they could. For example, we have seen doctors perform some tasks that are typically a prerogative of nurses as part of our collective effort to reduce the number of touchpoints with Covid-19 patients and, therefore, limit the staff’s exposure to SARS-CoV-2 and optimize the amount of PPE used without decreasing our quality. Also, since the pandemic began, standardization has allowed us to make correct use of our PPE stock in every single corner of the hospital and never run out. (In fact, we consumed more in March, when we were early into the curve and only admitted one Covid-19 patient in the entire month, than in the October peak, when we were receiving 150 suspected Covid-19 cases per day). Simply put, I don’t know how we would cope with this emergency without lean.
Lean has been fundamental to our transformation and successes since we started our journey nine years ago. We, therefore, encourage every healthcare organization in the world to explore all that lean can provide, to improve their processes, patient outcomes, and satisfaction of both staff and patients.
This article was originally published on Planet Lean, with the headline “Becoming a role model,” on February 15, 2021, and posted with permission.
Managing to Learn with the A3 Process
Learn how to solve problems and develop problem solvers.


Very good