The Lean Enterprise Institute’s webinar “A Roadmap to Lean Healthcare Success” with John Toussaint, MD, CEO of the ThedaCare Center for Healthcare Value, drew thousands of Lean Thinkers from North America and around the world who had more questions than we could answer in 60 minutes.
Most of the questions fell into several themes such as leadership, sustaining gains, involving people, and the A3 management process. What follows are your questions representing those themes and Dr. Toussaint’s follow-up replies.
Dr. Toussaint will go into even more details about lean healthcare at the 4th Annual Lean Healthcare Transformation Summit, June 5-6, 2013, in Orlando, FL.
Q: The “lean” approach can be difficult to sustain. Could you comment further on the challenges of realizing both the structural and cultural change needed to sustain a lean, QI culture?
A: The lean methodology involves people and processes which are tied together by the lean management system and oriented toward a specific purpose. All four puzzle pieces (purpose, process, people, and the management system) must be in place for success. Get the purpose, process, and people right without the management system, and the organization won’t sustain the lean effort. This is why we are so focused on teaching the management system here at the Center.
Q: How did you address the issue of having excellent, skilled providers who just won’t “get on board” with lean?
A: I always asked “what’s in it for the staff to do this”? Can we fix some of the problems faced by frontline staff members and physicians, for example? These may have been problems that existed for years. Once we fixed on-time starts in the cath lab, the cardiologists came back for more. Over time, they became some of the biggest advocates for the process improvement associated with lean.
Q: What does the term “gemba” stand for?
A: Gemba is the Japanese word for where value is created for the customer. It literally is “the place” where the work is actually done. In healthcare it would be in the clinic exam room, operating room, or emergency room.
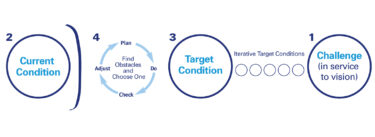
Q: We have trouble getting past the current state of an A3 because of a lack of knowledge of how to collect data. Do you have any suggestions?
A: Taiichi Ohno once said, “I like data but I like facts better.” Of course what he meant was that the real information you need is at the gemba. We all need to go, see, ask questions, and show respect to people. The dialogue that occurs there will be much more informing than any data we derive from the computer. The other point is that the A3 process is all about dialogue and teams developing an agreed upon understanding of what the real problem is. Data may be a tool to support that discussion but what we are really doing is thinking differently about problems as we let frontline team members shape our understanding of the actual reality of the work.
Q: What is the best way to engage senior executives in changing their own behavior?
A: I think there are several ways: 360 degree feedback from subordinates and peers is important to change behavior. If everyone on your team thinks you’re a jerk, it’s unlikely you will motivate them, let alone implement lean. A3 thinking is the management tool that builds a team. This is critical for senior executives to learn and should be one of the first priorities for their education. Finally, they have to go to the gemba. A lean facilitator should be with them to teach them how to begin to see waste.
Q: Could you say more about True North?
A: These are the small number of metrics that the senior team is responsible for developing. In healthcare we have too many metrics. Too many metrics confuse our staff. Senior management needs to choose five or six that really matter and deploy them throughout the organization. Everyone should be working toward the same performance metrics and they should be everywhere in the organization clearly displayed.
Q: Have you found people reluctant to bring problems up to management for fear of reprisal? If so, what have you done to counteract this?
A: We had to build a culture of continuous improvement. It didn’t happen overnight. Managers have one main responsibility, which is to mentor facilitate and teach staff how to identify and solve problems. In 2011 at the urban hospitals at ThedaCare there were 9,500 hundred staff ideas implemented. In 2012 there were 22,000 this year the goal is over 40,000. Release the creativity of thousands of people and these are the results you can achieve.
Q: Can you talk about how lean can help healthcare providers/professionals/caregivers deal with and react to the Affordable Healthcare Act?
A: Revenue is decreasing from the government payers and commercial payers are following suit. Lean is an operating system that when implemented successfully leads to better quality, lower cost, and more engaged staff. In a world where caregivers are challenged to do more with less, implementing lean is a great strategy.
Q: Two questions (1) Do you look at the cost / benefit on your A3’s. (2) How do you integrate ROI with the lean philosophy
A: I don’t believe in doing ROI on lean projects. The literature suggests there is a 3:1 return on investment in healthcare. In manufacturing it’s as high as 8-10:1. You must decide how you will prove whether lean is working. For me it was simply improved operating margin, improved cash flow, and improved productivity year-over-year system wide.
Q: How do plan for continuous improvement? Once you implement a project, how to make sure it stays on track? Being in process improvement, you are not the direct supervisor and it becomes hard to keep things on track.
A: If you don’t have a lean management system that supports continuous improvement it won’t sustain. Follow this link to learn more. http://www.createvalue.org/
Q: What is standard work for leaders?
A: I think there are a critical few standard work items for senior leaders. It includes hoshin kanri, A3 thinking, setting True North metrics, going to the gemba, and establishing a lean management system. This means the senior leader becomes a mentor, facilitator and coach. This standard work requires behavior change in leaders because most don’t have the humility and perseverance to learn an entirely new management system.
Q: Does ThedaCare have a regular “touring” schedule for outside companies to visit and see what good looks like? I am a project manager for a company located in Milwaukee, WI, and would be very interested in arranging a visit for myself and fellow leaders. That is one of our weak points in implementing lean within our company at the moment. We started almost a year ago.
A: We offer site visits twice a month go to www.createvalue.org to learn more. You will also see information on our summit June 5-6. 2013. The best lean healthcare organizations in North America will be there presenting. Have your executives rub shoulders with them.
Q: Thank you, John, for the great example ThedaCare has set for all of us!Question: Can you briefly explain “a day in the life of a ThedaCare RN?” How much time is spent at the bedside, how much time are they given to participate on improvement teams, how much time for education/training to improve their skills and problem solving? Do the RN’s typically work 12 hours shifts?Thank you!
A: RNs at ThedaCare are process owners for the inpatient experience. They typically have a team of five LPNs and clinical technicians that work with them and do most of the patient care including medication delivery, etc. RNs work 12 hour shifts. The RN, MD, pharmacist, and social worker meet as a team before seeing the patient each day and then examine the patient together as a collaborative team. RNs teach improvement as well as doing improvement. In fact, most say that improvement is the work. Identifying and solving problems at the frontline every day is the main activity of all staff not just RNs. To see a video of Collaborative Care, click on this link http://www.createvalue.org/resources/videos/collaborative-care-clinical-trio/
Q: In manufacturing, each value stream has a value-stream owner. Most manufacturing plants have just a few value streams. In a hospital environment, it seems that there are many value streams. How many value streams does a ‘typical’ hospital have and what level of management is assigned with the task of value stream manager?\
A: We are moving to “Enterprise wide value streams”. This maps the entire patient experience across a specific disease such as cancer. There are 23 “verticals” or departments a cancer patient has to navigate. We have put in place VPs for the Enterprise wide value streams similar to what Toyota does with their products. It’s a grand experiment to see whether in healthcare we can break down traditional structures like hospitals and clinics and create a perfect patient experience.
Q: You mentioned that most healthcare clinics have hundreds of performance metrics. You also emphasized how important it is to narrow down to very few. Could you list 3-4 performance metrics that you think are most important among those hundreds?
A: Preventable mortality, 30-day readmission rate, and gross revenue per full-time employee (productivity) would be examples.
Q: How much time should the CEO spend on the GEMBA in your opinion?
A: I was there one day a week for a couple of hours. The more the better though. Target getting to everywhere in the organization over a year and develop standard work for what questions you ask. Also go by yourself and don’t tell anyone you are coming!
Q: How many hours of formal training did your managers at ThedaCare get on lean framework and methodology?
A: Today managers receive four months of on-the-job training. This extensive training has basically eliminated turnover.