Ten years ago this month I made a visit to the Mayo Clinic’s large medical complex in Rochester, Minnesota. I was not there as a patient. Instead I was a sort of lean anthropologist. I was making my first foray into a major medical organization to examine its thought process and behavior from a lean perspective.
The trip was arranged by Dr. Don Berwick, the founder and president of the Institute for Healthcare Improvement in Boston, who had just convinced me that I should start LEI as a replacement for my former home at MIT. Don asked me to ponder a simple question: How would a major medical system go about implementing lean thinking across all of its activities? (As Don put it, “In healthcare we have no Toyota to copy. We don’t even have a Yugo. So where do we start?”)
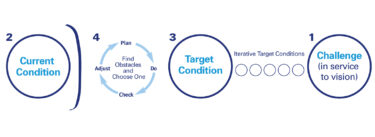
As always, I took a walk. Over two days I followed a number of patient pathways as well as pathways for medical supplies, patient schedules, and specimens going through the laboratories. (Lean Thinkers often call these pathways value streams.) And I soon reached a diagnosis: Severe sclerosis of patient and support pathways.
At Mayo (and in the many medical organizations I have visited since), I found brilliant doctors who were point optimizers, focusing solely on their narrow activity without much thought (or patience) for how it meshed with the other activities around them. The hospital’s administrators, by contrast, were asset optimizers, trying to keep every expensive machine, hospital room, and specialist busy, even if this meant delays for patients and heavy burdens for staff. The nurses were the members of the organization thinking about patient pathways and about core support processes like handling supplies and drugs. But they were doing this intuitively and reactively to somehow keep things moving. They lacked recognition of the importance of their task and a rigorous methodology.
Together, the brilliant doctors, diligent administrators, and long-suffering nurses were providing healthcare that cost too much, took too long, and often produced less than optimal outcomes. To make a lean leap everyone in the organization would need to change their way of thinking and acting.
My prescription was very simple: Identify all major patient pathways as well as support streams. Map them from end to end. Then ask how each pathway can be cleared of its blockages, backflows, and cul-de-sacs for the benefit of the hospital, its staff, and its patients. Finally, and most important, ask what changes in organizational lifestyle will be required to keep the pathways clear.
What troubled me was not the diagnosis or the prescription. I was pretty sure I was right. What I worried about was the prognosis. My recommendations would require everyone — doctors, nurses, and administrators (and suppliers too) — to change their behavior and organizational lifestyle. And as medical professionals know, lifestyle change is usually the hardest part of any treatment.
Given the difficulties involved, I ended my first venture into healthcare in May of 1997 thinking it was premature to hope for much progress toward lean healthcare. And I didn’t return to Mayo for ten years until last week when I spent a day with Dr. Henry Ting, a cardiologist with a natural instinct for process thinking. We looked carefully at the work his team has done recently to speed patients from the point they suspect they might be having a heart attack — usually far from a hospital — to the point where all appropriate treatments have been applied.
The results are quite dramatic. Rethinking this pathway saves lives — many lives — because the more quickly appropriate treatments are applied the more likely the patient is to survive and to survive without major heart damage. And here’s the really encouraging news: A lean pathway reduces costs for the hospital and makes life better for the staff. It’s a win-win-win. My skepticism on my previous visit was replaced with hope after this visit.
But I also realized while flying home that Dr. Ting’s team had performed a brilliant procedure on one of the easier problems to fix and sustain. They had analyzed a single pathway and one where the value of saving time is so overwhelmingly obvious that any medical organization will find it hard not to change its behavior once the sclerotic state of the existing pathway is clearly revealed. (Fortunately, their work is now being successfully paralleled throughout Mayo’s cardiology practice and by similar pioneers along other pathways in many healthcare organizations across the world.)
The hard part for all of us is to tie together these pioneering, single-pathway efforts — which seemed beyond our grasp only 10 years ago. We need to create a complete lean enterprise in which all pathways have been permanently cleared and the lifestyle of the organization has been changed as well. This will require more than lean techniques. It will require new management methods and a new type of leadership.
Given the urgent need for this lean leap, I’m truly delighted that my long-time co-author Dan Jones has taken on the challenge of asking what a truly lean healthcare system will look like. He is leading the first Global Lean Healthcare Summit in the UK at the end of June in which we will be asking what kind of leadership and what kind of management will be required.
We have invited doctors, senior administrators, nurses, and suppliers to describe the challenge as they see it. We will then work together to develop hypotheses about creating lean healthcare on a systemic basis that we can all test.
The most gratifying aspect of the recent embrace of lean thinking by the healthcare community — making the upcoming Global Lean Healthcare Summit possible — is that these are the most important value streams in our lives. Indeed, they often determine the length and quality of our lives. As I told an Australian healthcare audience recently, “Toyota takes better care of car parts than most healthcare organizations take of their patients.” And this is not right! We know how to do better and have a moral obligation to do so.
So I’m deeply encouraged that Lean Thinkers in the healthcare community are at last tackling the world’s most important value streams. But I’m also concerned that we will stop short with single pathway interventions. And I’m worried that improvements in individual pathways can’t be sustained because the organizations in which they reside have not changed. What the patient — the whole healthcare system — really needs is to think through the entire system from a management and leadership perspective so we can truly create and sustain lean healthcare.
Best regards,
Jim
Jim Womack
Chairman and Founder
Lean Enterprise Institute
P.S. I hope I will have a chance to meet many Lean Thinkers from healthcare and supplier organizations at the Global Lean Healthcare Summit in the UK on June 25 and 26, 2007. Please go to www.leanuk.org for details and to register.