When Dr. Sami Bahri opened his dental office in Jacksonville, FL, in 1990 he had two dental chairs, one assistant, a small front desk, and a gnawing hunch that the traditional way of running a dental office was full of waste. Just two years later, Bahri had five chairs, five assistants, three hygienists, a receptionist, a bigger front desk, and an absolute conviction that traditional dental management produced bottlenecks, wasted time, underused capacity, and created frustration for dentists and patients.
In the two intervening years, Bahri’s gut feeling that there had to be a better way had driven him to study a shelf-full of management books about continuous improvement. He had come to the conclusion that dental management schools, like their counterparts in business, had made some fundamental misjudgments about the best ways to manage office work. One of the shared misconceptions, Bahri believed, was the traditional view that batching — grouping activities by type — was always the most efficient way of organizing work. Schools taught dentists to batch similar procedures when treating patients to limit the time-consuming setup of instruments and materials that are performed to switch from one dental procedure to another. Thus, if you need two fillings and two crowns, your dentist schedules the fillings for one appointment and the crowns for another. Batching avoids setups but, as Lean Thinkers know, usually leads to more waste.
The traditional dental office also has a departmental “wall” between dentistry and hygiene. Dentists and assistants treat patients in dedicated dental chairs; hygienists clean patients’ teeth in dedicated hygiene chairs. Part of the reason for the distinction is due to tradition, part is due to the time needed to perform the setups between procedures, and part is due to the hour that normally is allocated per cleaning. As a result, patients move back and forth between “departments.”
Scheduling their movements is the job of another department, the front desk. In the traditional dental office it is the central point for collecting and distributing all information. This role turns the desk into a bottleneck as patients arriving and leaving every hour schedule new appointments, change existing appointments, make payments, and ask questions about insurance. Desk staff also updates dental charts, answers inbound calls, and makes outbound reminder calls. When Bahri was building his Jacksonville practice, the office stopped if his sole receptionist called in sick. “Some days I worked for free because I had no one to check out patients and take payments,” he recalled.
Looking for Alternatives
With traditional office management techniques “everything seemed so out of control,” he concluded. “But what could I do?”
At the suggestion of a fellow doctor, who had applied some total quality management (TQM) principles to manage a hospital emergency room, Bahri investigated applying TQM to dentistry. “I tried applying some of [W. Edwards]Deming’s statistical process control principles to my practice, but I didn’t feel it was improving a lot so I kept studying and looking for books,” said Bahri, who emigrated from Lebanon in 1990, where he was a founding director of the School of Dentistry at the Lebanese University
By the mid-1990s, Bahri’s bookshelf was a record of the era’s quality fads with works by Philip Crosby, Tom Peters, Michael Hammer, Steven Covey, Michael Gerber, Eliyahu Goldratt, and Peter Senge. He dedicated time every Thursday to teach office staff TQM concepts and cross-training. Dental assistants and hygienists learned front desk duties or how to answer common questions about insurance. Front desk staff learned how to set up cubicles in between procedures. His reading and cross-training resulted in some improvements to isolated processes but no overall dramatic improvement in how the office ran. Then in 1993, his reading led him to Masaaki Imai’s Kaizen that described TQM as well as the Toyota Production System. “The book was a smooth transition between TQM and TPS,” said Bahri.
As he implemented key lean production concepts in dentistry, he was struck by the importance of continuous flow while listening to a tape of Lean Thinking (Simon & Schuster, 1996). “I stopped the tape and started thinking, “That’s what I needed,” Bahri recalled. He read books by Taiichi Ohno, Shigeo Shingo, and other Japanese authors, studying all the lean tools from Five Ss to total productive maintenance. He was most impressed by the single minute exchange of die concept for slashing setup times. “I was very impressed by reducing setup time,” he said. “It was the heart of establishing flow.”
Dentistry as a Job Shop
Setups are almost as common and just as wasteful in the average dentist’s office as in the average factory. Just as a factory stops a process to “set up” or change tools and materials when switching between different jobs, dentists stop to change instruments and materials when going from one procedure, such as a filling, to a different one, such as a root canal.
In manufacturing, mass production thinking told managers to schedule work in large batches to make up for the time lost when equipment was stopped for setups, which could take hours. The problem from a lean thinking perspective was that large batches led to a host of wastes that were collectively much worse, such as overproduction, long lead times, poor response to changes in demand, and long waits between processes as products waited for the next department to finish its big batch and changeover.
In dentistry, conventional training told dental students to schedule patients by batching like procedures to avoid setups. “When I made your appointment I would see how many fillings you had and I scheduled them together,” said Bahri. “I had a different setup for crowns so the next time you came, I would do the crowns. Most of the time, dentists tried not to switch from one type of procedure to another in the same appointment because of the time that it takes to do setups.”
He estimated the typical dental setup of preparing tools and materials takes about 15 to 20 minutes. Thus, a patient needing a root canal and crown even if they are for the same tooth will need a separate visit for each procedure. “The problem is that in your mouth, you need crowns, fillings, root canals, veneers, etc.,” Bahri said. “So when you come to me, I should have the flexibility to go from one to the other nonstop. That puts the mouth at the center of the process.”
Batching dental procedures avoids setups but leads to other wastes. For instance, if you arrive for a dental appointment needing a procedure other than the one scheduled (like a root canal instead of a filling) the tools and materials for the scheduled procedure must be removed while tools and materials for the new procedure are set up. Even if the appointment goes according to plan, traditional scheduling extends treatment time. For example, if you need a root canal, two fillings, and four veneers, you’ll need at least three appointments. That means three roundtrip drives to the dentist, three periods away from work or leisure, and three times the chance that at least one appointment will have to be rescheduled.
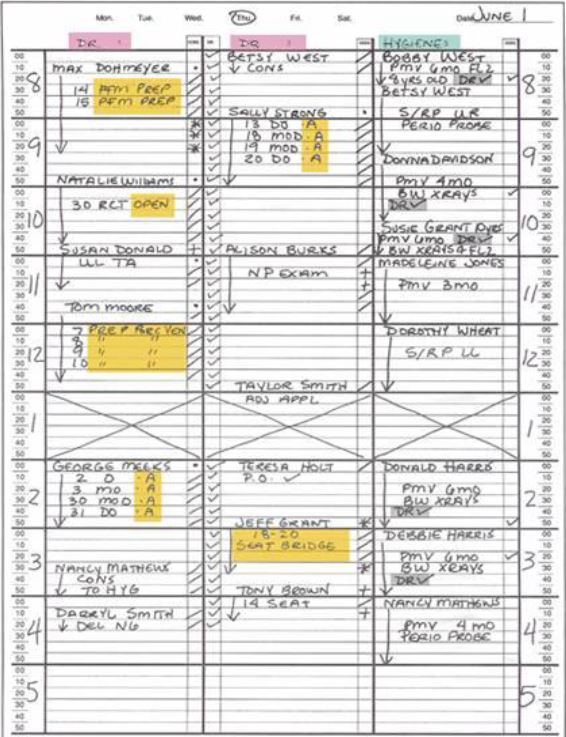
This schedule shows work organized by batch and function in a typical dental office. The hygienist’s chair (right column) is scheduled separately from the two dental chairs. Note how dental procedures are batched. The “A” for amalgam shows a series of fillings scheduled for patients at 9 a.m. and 2 p.m. Source: Appointment Scheduling by James Pride.
Bahri saw other parallels between industry’s traditional mass production thinking and the traditional thinking about how to organize dental work. A traditional mass producer groups machines by functions: the milling machines in one department, drills in another, grinders in another, etc. Production control schedules the movement of batches of parts from one functional department to another, creating waste every step of the way from overproduction, undiscovered defects, and unnecessary transportation to name a few.
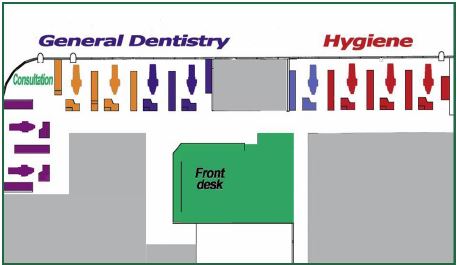
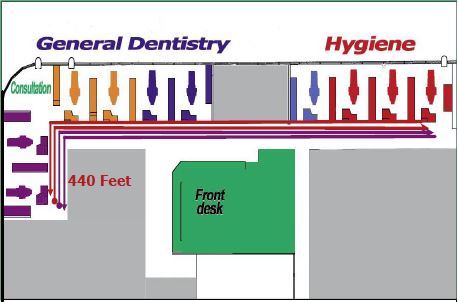
Bahri’s original office, like a factory, was organized by functions. He and two other dentists along with their assistants worked in the dental “department,” a row of treatment cubicles dedicated to dental procedures at one end of a hallway. At the other end, hygienists worked in a row of cubicles with chairs dedicated to hygiene.
“It was organized like mass production. I wanted to change that,” said Bahri, who has been recognized as “the world’s first lean dentist” at a Shingo Prize conference. “I don’t think healthcare professionals realize how much their offices are influenced by mass production assembly lines. Lean principles identify activities that consume time or other resources but don’t add value from the patient’s point of view. By removing these wasteful activities, a lean transformation gives healthcare professionals more time and resources to spend on personal patient care.”
Starting the Lean Journey
Bahri suspected the departmental arrangement created a lot of walking and delay as hygienists walked 100 feet from their end of the hallway to the dental chairs at the other end to tell a dentist that a patient was ready for an exam or a procedure. Curious, he observed conditions and drew a simple chart. It showed that a hygienist usually made two trips back and forth before the dentist was free to examine the hygiene patient down the hall. After walking to hygiene, the dentist walked back for his or her next dental patient. “We walked a total of 600 feet to check on a patient,” Bahri said. “This chart was a very good tool to convince staff about waste in the office.”
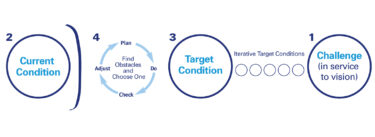
From his study of lean thinking, Bahri believed the solution was to introduce flow, being able to move from one procedure to the next — from hygiene, to root canal, to filling. To do it, he’d have to break down the functional wall between hygiene and dentistry. That breakthrough relied on dramatically reducing or even eliminating setups in between procedures. The potential benefits were huge for patients, staff, and dentists. Consider the steps in a typical visit:
- Check in the patient
- Seat the patient
- Numb the tooth and surrounding area
- Prepare tooth for treatment
- Take x-rays
- Treat the tooth or gums (From the patient’s perspective, this is the only value-adding step!)
- Collect payment
- Update dental chart
- Schedule next appointment
Imagine a patient needing three office visits to complete a treatment plan. The same nine steps are repeated for each visit, but only one, step six, adds value. If the dentist and hygienist could complete all the value-adding work in one visit, the patient does the first five steps and the last three only once instead of three times. The only possible downside, Bahri thought, was that patients would have to spend more time during one visit to have all value-adding work performed. A single visit could last from one hour for simple work (filling and a cleaning) to three or four hours for more complex work (multiple fillings, root canal, and crown). But Bahri bet patients would like the change. They’d save time, travel, and the hassle of scheduling and rescheduling visits. Most importantly, Bahri noted, a patient’s mouth would be returned to health much faster.
For Bahri and staff, collapsing multiple visits into one or two also meant less waste: fewer appointments to book or reschedule, fewer outbound reminder calls to make, fewer setups, etc. The enabling step of eliminating setups would clear the way to do hygiene and dental procedures in one chair. It had the added benefit of freeing capacity by making hygiene chairs available in the same office space for more dentists to join the practice, bringing in additional patients and revenue.
Standardized Setups
The key to dental setups are cassettes, sterilizable metal trays holding as many as 30 instruments (see photo at right). Each procedure, such as a crown, filling, root canal, veneer, extraction, has its own setup cassette. Bahri began noting just how often tools in the various cassettes actually were used.
After several months, he and the other dentists in the office realized that 90% of the work they did required 10 or 11 instruments. “Among the doctors here we have all agreed on certain instruments that we all need and we’ve standardized the cassette,” said Dr. Komal Relan, a dentist in Bahri’s practice. She estimated that specialized instruments were needed “less than 10 percent” of the time. These instruments were put in sterile pouches and kept nearby in the cubicles for when they were needed.
A standard cassette for all procedures eliminated instrument setups, but there still was the problem of material setups. Before each procedure, assistants prepared the working tabletop with materials taken from a plastic tub in each cubicle. The tubs, in turn, had to be stocked with inventory kept in a storage room with several rows of shelves. Besides tying up money, the large amounts of inventory meant some material inevitably became very expensive waste because many dental materials, such as anesthetic solutions, have expiration dates. “After that you throw it away,” said Bahri.

Bahri replaced the boxes of inventory in the cubicles with “little supermarkets,” small racks of plastic trays holding small quantities of virtually every material needed for any procedure. “We put a little bit of everything in the cubicles so I can go from one procedure to another,” he noted. At first, dentists or hygienists wrote on sticky notes what materials needed to be replenished. They stuck the notes to the supermarket trays holding the particular material in short supply. At the end of the day, a part-time employee wheeled a cart stocked with materials from cubicle to cubicle, replacing what had been consumed. When the part-timer left, office staff created a new system. Every hour, an assistant working in a cubicle wheels the cart to the cubicle next door where the next assistant replenishes the small supermarket and, on the next hour, wheels it to the next cubicle and so on through the office. “We don’t know what the best system will be yet,” Bahri said.” A few cabinets with material for replenishing the cart have replaced the storage room.
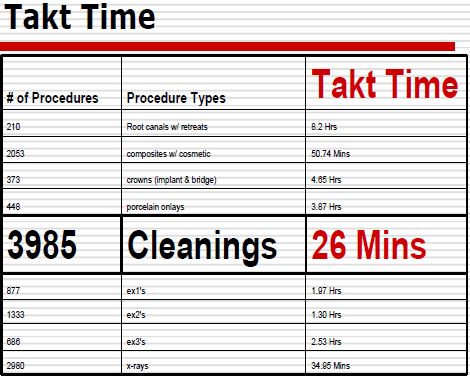
At about the same time he eliminated setups, Bahri analyzed an annual history of procedures performed in his office to determine what was done most often. Cleanings at 3,985 were the runaway winner. Dividing by this number the available work time of 104,160 min., the time the office is open during a year, gave him a takt time of 26.13 minutes. “Every 26.13 minutes we had a cleaning ordered,” he said. Despite this stable average rate, the workload of hygienists varied greatly day-to-day. Some days the two office hygienists didn’t have enough work to keep them busy; other days Bahri had to bring in a third hygienists to help.

“The next question was, „How long did it take to do a cleaning?’ ” Bahri said. Using takt time and cycle time data, Bahri could calculate the number of hygienists actually needed to meet the rate of demand for cleanings (the takt time) instead of applying the traditional dental management formula of having one or two hygienists per dentist. He also would be able to distribute cleanings evenly throughout the schedule, eliminating the “peaks” and “valleys” of too much or too little work for hygienists to do.
Equipped with a stopwatch, pencil, and paper, Marisa Young, an office flow manager, studied hygienists working. She and Bahri discovered that a cleaning could be done in 20 minutes, six minutes less than the takt time, after nonvalue adding activities, such as walking to dentists’ cubicles and cleaning up between patients, were eliminated. Dental assistants and two “flow managers” took over the hygienists’ jobs of cleanups, collecting payments, presenting treatment plans, and making appointments.
“Every 26 minutes a cleaning was ordered so hygienists had six minutes of free time in between cleanings, which is okay with me,” Bahri said. “It can’t follow the same drumbeat as an industrial process. And at that time, I was allocating an hour for cleanings, so I had cut it by half.”
Next, he asked, “How many cleanings do we need to do per day to cover the 3,985 ordered annually? The answer was 12 cleanings.” That meant the office’s two hygienists each had to work three hours per day to cover 12 cleanings, not the seven hours apiece that had been allocated. At that rate, hygiene treatments could be combined with dental procedures in one chair.
Bahri did a pilot project with a hygienist to test the idea. Patients who were due or overdue for cleanings were identified on the office schedule. When they came in for a filling or other dental work, they were asked if a hygienist could do a cleaning. Most agreed because it didn’t require returning for another appointment. While a patient’s mouth was getting numb, the hygienist came to the chair, did the cleaning, and moved on the next patient before the dentist returned.
As a result of these key improvements — eliminating setups by developing a standardized cassette for all dental procedures, stocking small quantities of the materials needed for virtually all procedures at the point of use, and combining hygiene and dental procedures in one chair — most patients were getting all their dental work and cleaning done in one or two longer visits, instead of five or six. Because the office is much more flexible, many patients can be given same-day appointments for cleanings and other non-emergency procedures, said Bahri.
“It’s a total paradigm shift from what goes on in other dental offices,” said Dr Anjali Lueck, a dentist in Bahri’s practice. “We’ve taken the approach that when the patient sits down in a chair they can receive dental education, their cleaning, and any treatment because we are set up in each room to treat everything. As dentists it gives us better control over what we are doing. From a patient’s perception, it means fewer overall visits.”
Patient Jerry Bussell likes the changes. “You barely sit down in the waiting room and someone comes to take you in. I wait less than five minutes. It’s so unusual,” said Bussell who also likes having fewer visits.
Bussell had come into Bahri’s office for a checkup prior to a trip to Japan. When he mentioned he was visiting Toyota, Bahri showed him his library of lean books and workbooks. Bussell, a vice president of global manufacturing at nearby Medtronic where he was leading a lean transformation, invited Bahri to see the concepts in action at a Jacksonville plant.
“When I saw what Jerry had done in the factory, I was inspired,” Bahri recalled.
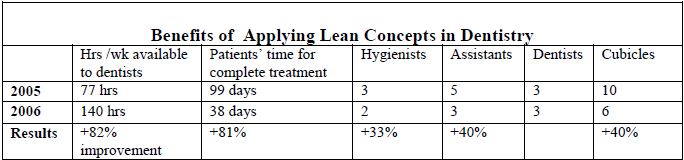
The box score above shows the advantages of implementing lean concepts in Bahri’s office. The same number of dentists needed less support but had more capacity. (When one hygienist left, Bahri didn’t replace her.)
Technology’s Role
Bahri integrated new technology slowly with the process improvements. Computers and printers installed in each cubicle eliminated backlogs at the front desk by decentralizing information processing. New patients use the computers to fill out information forms online in the cubicle where they will begin treatment. Dental assistants at the cubicles use the computers to take payments, discuss insurance with the patient, and make appointments. Patients leave without having to stop at the front desk.
“What Dr. Bahri is trying to accomplish here is that every room functions as an office so the patient doesn’t have to run back between the front desk, a hygienist’s chair, and a dentist’s chair,” said Dr. Relan.
Other capital improvements include digital x-ray machines to produce pictures in seconds, a scanner to capture images of insurance checks and benefits descriptions, and a small computerized dental milling machine that makes crowns in about 30 minutes. The machine allows crowns to be made during a visit by eliminating the need to send dental impressions to an outside lab.
Culture Change
The changes have altered staff roles. Candice Johnson was a treatment plan coordinator, taking diagnoses from dentists, entering them into the computer system, and presenting the plan to patients. Now she is one of two patient care flow managers. Basically, her job is to resolve any problems delaying treatment.
”We make sure when a patient is seated that everything runs smoothly from beginning to end,” she said. She has been cross-trained in all office procedures, including cleaning dental or hygiene chairs, taking payments, taking x-rays, or explaining insurance to patients.
A patient seated in the waiting room is a sign there is a problem. “If a patient is waiting to be seated, I’d pick up on that right away,” said Marisa Young, the office’s other flow manager. “I’d go and investigate to find out what’s going on. Maybe a room needs to be cleaned or instruments sterilized. Every minute the patient should have something valuable happening, not sitting outside in the waiting room.” She and Johnson spend most of their time on the office floor not behind the front desk, so they are available to answer patients’ insurance questions. They also watch for red cards posted atop cubicles. A dentist or hygienist who is falling behind schedule, displays the card to alert flow managers that they’ll need extra help to get back on schedule. Green cards hanging outside cubicles indicate “on time.” If a dental assistant is free, the flow manager asks her to help where needed. If all the assistants are busy, the flow manager helps.

Front desk assistant Christine Catlin now focuses mainly on outside customers, taking calls, making outbound calls to confirm appointments, or verifying and updating insurance coverages. She admitted being skeptical “at first” about all the changes. Now, she enjoys the new way of working, including the daily 8:45 a.m. meetings when Bahri and staff review the day’s schedule to anticipate possible problems and share improvement ideas. “It’s really neat because in a lot of offices the attitude is, „This is how we do things.’ But here, if you come up with an idea, we’ll try it. I actually I look forward to changes now.”
For More Information
Dr. Sami Bahri, DDS, Bahri Dental Group: http://www.bahridental.com