In the improvement world, Kata is the deliberately practiced thinking routine that turns repetitive mental activities into an unconscious meta-habit: A learner is guided by a coach (Improvement Kata) and answers a series of questions from the coach (Coaching Kata); a second coach frequently observes the learner/coach interaction and offers guidance.
With each brief but daily Kata routine (15-20 minutes), the learner uses experiments to identify and remove obstacles that keep them from reaching a target condition.
Over time the learner begins to detach from the rigid script and intuitively approach problems with the meta-habits embedded by Kata.
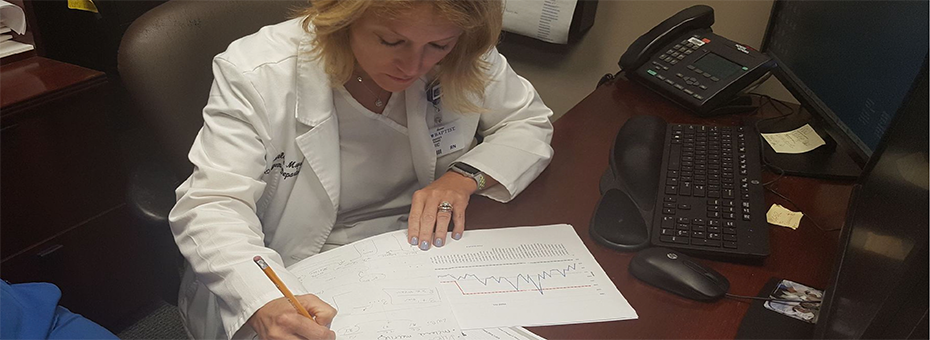
 Melanie Mays, Nursing Manager of the Baptist Memorial Memphis Hospital emergency department (ED), began to recognize her reliance on meta-habits after approximately six months of work as a Kata learner and coach. Her approach to a recent problem in the ED illustrates how she relied on meta-habits.
Melanie Mays, Nursing Manager of the Baptist Memorial Memphis Hospital emergency department (ED), began to recognize her reliance on meta-habits after approximately six months of work as a Kata learner and coach. Her approach to a recent problem in the ED illustrates how she relied on meta-habits.
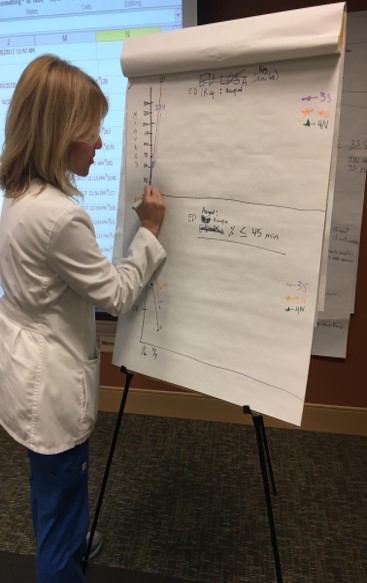
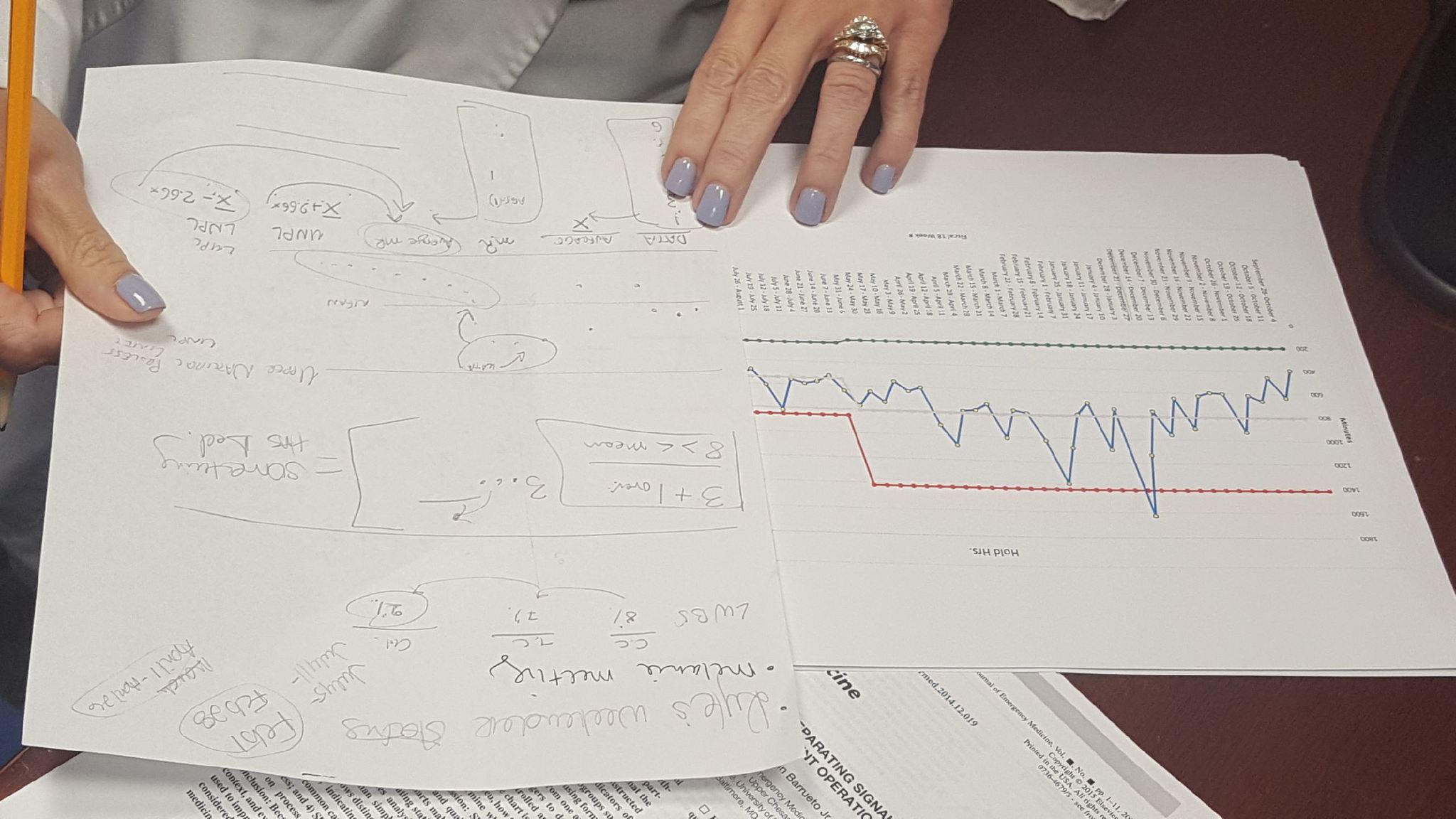
In late December 2017, Mays saw that flu cases were spiking in the ED, in part because the flu shot was not as effective as in past years. The increasing volume of flu patients (ESI Level 4 and 5 patients) was negatively affecting the patient length of stay (LOS) in the ED for all patients, both the flu patients and those with more severe conditions. Over three days, Mays instinctively and repeatedly worked to find and eliminate obstacles that were preventing a target condition of lower LOS in the ED and less spread of the flu virus within the ED:
- Day 1:Volume in the ED had increased by 18 percent for the month. One mid-week morning before the Christmas holiday, the ED was extremely busy. May assessed the situation — reviewed patient types, capacity, etc. — and noted that many were young patients with flu symptoms. She also knew it was necessary to get these flu patients out of the ED faster to reduce flu contact with other patients and staff. Mays spoke with the charge nurse and pivot nurse and decided that flu patients should not be taken back to the main ED but moved to an isolated area (a temporary flu clinic). And instead of using the ED’s tube system to transport flu swabs for testing, they would be manually taken to the lab to save time.
The new process was enacted immediately (an experiment), and helped to get the flu patients away from others and treated more quickly, but it also caused obstacles to emerge: More communication was needed with doctors and staff, who were not aware of the changes; time was being wasted moving patients to and from the waiting room; the flu area initially lacked necessary items (swabs, bags, oxygen sensors, dedicated computer, tissues, masks for staff, etc.); and, although faster than using tubes, time was wasted by walking the flu swabs back to testing. Mays took notes of what to change for the following day. - Day 2: The ED staff was now fully aware of the new flu clinic process, and the young flu patients were triaged initially only for oxygen and major medical information (other information was collected after the flu swabs were tested), and the flu patients were escorted directly to the flu area (they were not taken to the waiting room). All items were stocked in the flu clinic, physicians knew where to find patients when flu screens were returned, and Mays and staff were able to rapidly process the flu patients. A few obstacles still existed, however, such as delays in getting respiratory treatments for some patients and too much time waiting for lab workand flu tests to return.
- Day 3: After communicating with the respiratory department and the lab, all facets of the flu-patient process worked smoothly. The lab recognized and responded to the need for a quick turnaround and respiratory was able to provide breathing treatments during the nursing assessment.
Over the three-day span the flu patient LOS was reduced from 125 minutes to 30 minutes. The LOS for all ESI Level 5 patients was reduced from 111 minutes to 44 minutes. And the isolated process also reduced flu cases among ED staff and helped to prevent staff “call-ins.”
Over the three days that Mays was making changes, she did not go to the Kata storyboard (a whiteboard representation of the Kata routine that allows a learner to detail the pursuit of a single target condition) in the ED, as would be normal when working the Kata routine. She says it was actually set up for another target condition that was strategic to the hospital’s overall challenge. After the holiday break, the flu surge subsided and Mays went back to the board and documented everything they did, relying on the notes she had taken during the experiment with the flu clinic.
“We never thought we were going to change the Kata board to do this,” Mays recalls. “I didn’t have that idea until I looked at the overall impact of the Level 5s and how what we [did helped these patients and] brought down the discharge length of stay for the entire population. So that’s when we went back to the board and made that our focus process.”
The previous winter Mays had had a similar experience, and that’s when she began to notice her detachment from the basic Kata. Prior to then she relied on a plan to undertake changes, measure the impact, review results, and then consider the next obstacle to remove. She was repeatedly removing the next obstacle in a scientific manner, but it was not yet a meta-habit or muscle memory.
“It’s especially important in a hospital that you have that muscle memory,” she says. “We talk about processes a lot (in the ED). If you have a process, it frees your mind up to deal with the situation. If I’ve got to decide how am I going to do this and what equipment I need, then I am going to be wasting time and not doing it.” The first day with the flu clinic she was learning patient by patient, measuring times for activities, and studying flow, which revealed new obstacles to her. If she had not been tracking her experiment, Mays says, she might have thought the time for physicians to come to the flu room would have been the biggest delay.
When starting out with Kata, Mays recalls that she and others at Baptist Memorial Memphis Hospital were prone to list things that “bothered” them as obstacles or choose a solution or new idea before fully identifying the obstacles with the current condition. She now sees the need to experiment with a new process and allow it to surface obstacles before developing and testing a hypothesis. “You cannot put obstacles on the board until you go out and grasp the current condition and try to reach the target condition — the obstacles will be there, and then you list them.”
Improvement Kata/Coaching Kata
Develop Scientific Thinking, a Foundation of Lean Management in the 21st Century.