Continuous improvement efforts are most effective when people directly involved in the work develop solutions to the problems they deal with daily. In healthcare, the result is better patient care for less costs and increased job satisfaction for staff.
But how do you directly involve the staff at 60 hospital emergency departments scattered around a big state?
A team of eight independent facilitators working through the Michigan Hospital Association figured it out. They explained what they did in Perfecting Patient Journeys, a how-to guide for using lean management principles in healthcare. Two of the authors recently talked about the improvement effort to Paul Akers, founder and president of product development company FastCap, and host of The American Innovator show.
Judy Worth and Tom Shuker explained that it was impractical to bring teams from 60 emergency departments (EDs) to three-day lean training sessions or send facilitators to train on-site at each hospital. So the team of facilitators used a method they called value-stream improvement (VSI).
Value-Stream Improvement
Firsts, the facilitators created a collaborative by dividing Michigan, where all the hospitals are located, into eight zones with roughly five to 10 hospitals in each zone, Shuker said. Two to three representatives from each hospital ED met once a month to tackle the problem of how to reduce the average length-of-stay (LOS) for emergency patients who could be treated and released. Most teams focused on one part of a patient’s ED stay, typically the initial part, known as “triage or “door to doc.”
These representatives learned how to identify and select a problem for an improvement project, define the project’s scope, and create a shared understanding of what was occurring in the process. The main tool for this initial stage was value-stream mapping, a representation – often hand drawn — of every step in the patient and information flow of a process, along with key data.
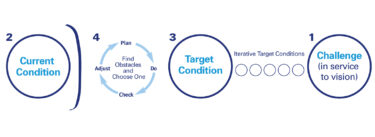
“From mapping we went to the value-stream improvement methodology,” Worth explained. “It really is a group problem-solving approach, not just current-state mapping but future-state mapping with an improvement plan for how you are going to start implementing the future state. And from there, we focused on rapid learning experiments and formal and informal checks and reviews. It really goes way, way beyond mapping.”
The methodology also included problem solving based on the plan-do-check-act process and visual management in the form of “huddles” or problem-solving meetings at project dashboards.
Worth said that the value-stream improvement approach also put a lot of emphasis on “socializing” improvement plan recommendations, a process for sharing knowledge and gaining acceptance of the recommendations. So at the end of meetings, hospital representatives got homework requiring them to explain to colleagues, including doctors and nurses, what they had just learned and solicit feedback on the suggestions.
At the start, Shuker said he was concerned about the cross-functional composition of the hospital improvement teams, which included not only doctors and nurses but staff from radiology, laboratories, as well as EDs.
“We were very much afraid it would be a finger pointing session, but within an hour everybody was focused on trying to layout the work as it existed and you could hardly tell what person was from which department. They were all trying to solve the problems in front of them.”
The problem in reducing LOS included myriad delays, work-arounds, and bottlenecks among other issues. “There was a lot of wasted effort and time,” said Shuker.
Participating EDs saw the number of patients who left without being seen drop by a nearly one-third. And the number of patients who left against medical advice declined by slightly more than one-third. Shuker and Worth said it would take more time to see an overall drop in LOS as teams continue to work on other parts of the ED value stream, such as discharge. Surveys of doctors and nurses revealed greater engagement in improvement efforts as a result of being in the collaborative.
Patient Focused
The value-stream improvement approach allowed everyone on the improvement teams to see the problems, measure the impact, and agree on solutions to quickly. “What we did thru this collaborative was flesh out ideas they could test with rapid improvement experiments,” he said.
In response to a question from Akers, Shuker said healthcare professionals were a “little hesitant” at first about applying lean concepts, which originated in manufacturing, but they quickly began working together to solve problems.
“Our phrase for it is see together, learn together, act together,” said Worth.
Akers said he liked the book “because it’s focused on the patient –the customer — not how the hospital makes more profit. If you put the patient first everything is going to take care of itself.”
The authors said Perfecting Patient Journeys is aimed at healthcare professionals in these roles:
- Unit, department, or value-stream managers, such as ED unit managers
- Senior executives who are improvement effort champions
- Continuous improvement facilitators
Perfecting Patient Journeys
- By Judy Worth, Tom Shuker, Beau Keyte, Karl Ohaus, Jim Luckman, David Verble, Kirk Paluska, and Todd Nickel
- Published February 11, 2013, by Lean Enterprise Institute, Inc.
- ISBN: 978-1-934109-36-6
- 161 pages, hardcover, illustrated
- $70.00; Discounts on purchases of 10+
- Media: Chet Marchwinski, cmarchwinski@lean.org, 617-871-2930
Download excerpts and read praise from healthcare professionals for Perfecting Patient Journeys at: https://www.lean.org/BookStore/ProductDetails.cfm?SelectedProductId=355&ProductCategoryId=9
- The American Innovator Perfecting Patient Journeys: Part one http://youtu.be/p5ttYNdE9m8
- The American Innovator Perfecting Patient Journeys: Part two http://youtu.be/z4pA4pudweI