What do you do when trying to get leaders who are generally resistant to change to engage in change efforts — especially when that includes standardizing their work? That’s the challenge Dr. Lynn Martin and the healthcare industry faces when engaging physicians in efforts to adopt new clinical protocols. In this webinar clip, Dr. Martin describes how he worked with physicians at Seattle Children’s to eliminate the opioid use in its ambulatory surgery center and make significant progress reducing their use in the more complex surgeries at the hospital. Find a lightly edited transcript below.
One of the challenges I’ve faced over the last 20-plus years as I’ve focused on quality improvement within healthcare is how do we go about standardizing a clinical process that involves physicians. And there are really, when you’re involving physicians, there are these five key points that you need to follow to develop standard clinical practice, or standards of care.
- Engage Staff: You need to engage the staff that are practicing in the development of those clinical practices.
- Observe the Actual Practice: You need to go and observe the actual clinical practice and all the variation inherent in that practice to learn from it.
- Make Evidence-based Decisions: You want to go to the published literature, what’s evidence-based best practice, and try to incorporate that into the protocol as you develop it.
- Make Consensus-based Decisions: Unfortunately for us, for most of what we practice, there’s not clear irrefutable evidence in the literature saying this is best clinical practice. So more often than not, you are left with a situation where the protocol is developed through a consensus-based decision-making. But again, it involves the frontline staff in coming to those decisions.
- Make it Easy to Follow: Once you’ve established a clinical protocol, a standard practice, it’s then incumbent upon the leader in that local area to really focus on making it easy to follow the protocol — [make it] easier to follow the protocol than deviate from the protocol is ultimately what I try to do
To achieve those goals, it’s typically most effective when the protocols are developed locally in local work units. And, ideally, to facilitate compliance with those protocols, you want to embed them into the electronic health record as much as possible.
Engage the Staff
You can see step number one is staff engagement. So, how do we talk about and how do we focus on engaging staff? Well, ideally my approach is, as a leader in a work unit, I say here’s a problem we, as a group, need to address, is there anyone interested in working on that problem? I seek volunteers and typically those volunteers are change agents, so to speak. They typically are more accepting of change because they’re typically frustrated with the current practice. Having someone who volunteers to participate, a peer, is a critical step in getting engagement of the others around them.
The next step for that volunteer is to observe peers in practice and then complete that literature review, looking for that best evidence, creating the draft of the protocol, the guideline of care that they’re trying to create. And, then they present that draft to the group for discussion, and then ultimately through a consensus tool, the group comes to a consensus and agrees to the protocol that they will then follow and use for further improvement.
Many physicians may practice in a silo; they practice one-on-one with their patients, and they have very little knowledge about what’s going on around them and how their peers are actually practicing. So, you really almost have to teach the physician peers how to go and observe the clinical practice; what are the key elements? So, we teach them to clearly define all of the steps in the process or the procedure that they’re looking at. They need to note the sequence of steps. Then ideally when there’s variation in the steps, identify where that variation occurs in both content and sequence.
And ideally we help them draw a simple little map of what that current state process looks like. And, and then, through the protocol that they draft, what their target condition process map would look like.
Virtual Lean Learning Experience (VLX)
A continuing education service offering the latest in lean leadership and management.
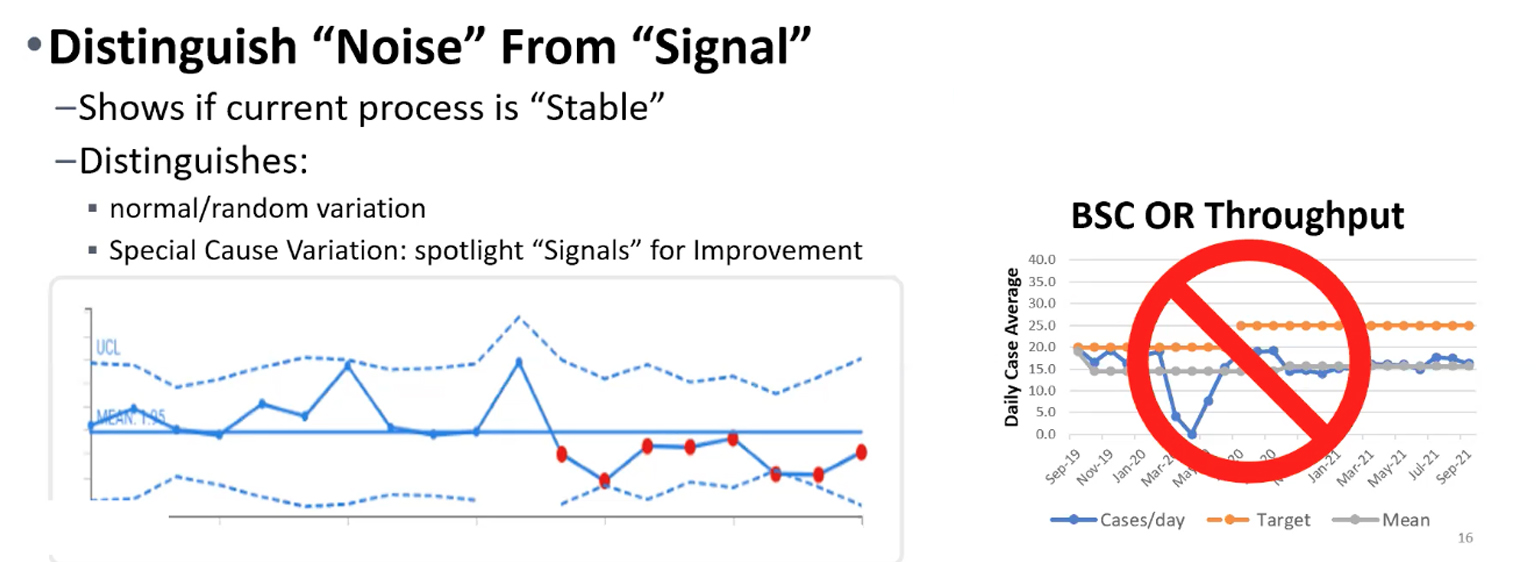



I’d love to hear more about their use of SPC Charts / Control Charts as illustrated in the photo up top. As it suggests, when we’re measuring improvement, we have to be able to distinguish between “noise” in the metric vs. real statistically-meaningful levels of improvement.
SPC Charts (aka “Process Behavior Charts” as Prof. Don Wheeler calls them) are incredibly useful in helping us understand cause-and-effect relationships between attempts at improvement and our key measures.
If you make a change to your system and the next data point(s) are within the range of “common cause variation,” then you might not really have evidence of meaningful improvement. You’d want to see a “signal” in the SPC Chart — something that indicates that the metric is no longer fluctuating around the baseline average level / range of performance.
Here is a related article that I wrote for LEI: https://www.lean.org/the-lean-post/articles/react-less-and-improve-more-by-using-spc-more-effectively/