Lean management case study series
Akron Children’s Hospital (ACH), a regional pediatric care system headquartered in Northeast Ohio, could be compared with David, the young lad who courageously brings down a giant in a classic Old Testament tale.
In this story, though, David battles two giants.
Akron is about 35 miles south of Cleveland, where two nationally ranked pediatric hospitals draw families from around the world who need specialized care for their children’s complex medical problems. Parents are attracted to the hospitals’ international reputations for being among the best: The Cleveland Clinic’s Children’s Hospital and University Hospital’s Rainbow Babies and Children’s Hospital are known for breakthrough research, life-saving surgeries and treatments, and other medical innovations. They also aggressively recruit gifted doctors, leading scientists, and other medical experts at the top of their professions.
But ACH, which certainly has a stellar regional reputation, is taking a unique weapon into the field as it battles for a bigger slice of the state’s pediatric care market. While the two Cleveland hospitals have continuous-improvement programs, neither has made continuous improvement a strategic imperative across its entire enterprise as ACH has.
The hospital’s Center for Operations Excellence (COE) is the engine that propels all employees and functions toward the growth goals set by executives and board members in hoshin kanri (strategy deployment) planning. Leaders are confident that the COE and its lean six sigma-focused training and project leadership give ACH enough competitive advantage to succeed, even in the same geographic market as two healthcare giants.
ACH’s expansion plan includes increasing the number of patients served both geographically and within certain sub-specialties; becoming the No. 1 choice for parents and referring physicians through quality achievements and availability of services; improving on infrastructure, quality, and clinical programs; and becoming the primary site for pediatric medical research in Northeast Ohio.
Already, the three-year-old COE has been widely embraced and highly effective. Projects have saved ACH millions of dollars, increased utilization of expensive assets, and reduced wait times and processing for patients and their families. The short-term gains are important, said Doug Dulin, the COE’s senior director, but the learning and commitment that each project builds internally are more crucial.
“What it comes down to is that we have to create a competitive advantage,” said Dulin, who learned the Toyota Production System at Aoyama Seisakusho, a Tier One supplier to Toyota Motor Manufacturing. “So how can we transfer what we’ve already done into every segment of the hospital? That’s how the Center for Operations Excellence fits in. This is a long-term journey.”
Akron Children’s Hospital at a Glance
- Largest pediatric healthcare system in northeast Ohio.
- Operating two freestanding pediatric hospitals and offering services at nearly 80 locations.
- Pediatric specialties draw half a million patients annually, including children, teens, and adults from all 50 states and around the world.
Level-Loading Schedule Improves Quality, Access, and Revenues
In addition to the challenge of having two highly regarded competitors in the market, ACH must do much more with much less. It doesn’t receive the numerous large grants and donations that the others do; and since all of the hospital’s patients are children, it can’t rely on Medicare reimbursements. Also, both the Clinic and UH are closely aligned with Case Western University Medical School in Cleveland, and so have access to more intellectual property, research programs, emerging technologies, and other assets than ACH has.
The hospital system’s smaller and less complex operation, however, seems to have been an advantage for quickly absorbing the lean culture. Evidence of how open all levels of the organization have been to lean is the speed with which a large number of employees — including doctors — have come together to identify problems, find the root causes, and then agree on countermeasures.
“There’s something about the culture at Children’s that allowed this to be very effective, very quickly,” said Board Member Bill Hopkins. “They were just primed for this. It speaks volumes about the commitment from everybody — the leadership, staff doctors, nurses.”
For example, MRI scheduling was one of the first areas the COE addressed because it had potential for significant and fast improvement, and because the hospital had not been able to effectively utilize a second MRI machine it had purchased. The most apparent barrier was a bottleneck in scheduling.
A kaizen event revealed that variability was the root cause: Children are more prone to move during exams when they need to be still, a reality that extends their appointment times because readings frequently need to be delayed or redone. On any given day, more than half of the hospital’s patients are five-years-old or younger, and so are particularly prone to moving during exams. Some children need to be sedated to keep them still. This causes more variability because a doctor needs to administer the sedation, and doctors’ schedules routinely change without notice because of emergencies and other unexpected events. The result was a backlog of patients with appointments, and long wait times for those needing new appointments.
The two-day kaizen — which included radiologists, radiology technologists, schedulers, nurses, and the employees who handle insurance authorization and registration — produced multiple solutions:
- Modifying the master schedule.
- Streamlining the insurance authorization process.
- Implementing standardized work instructions.
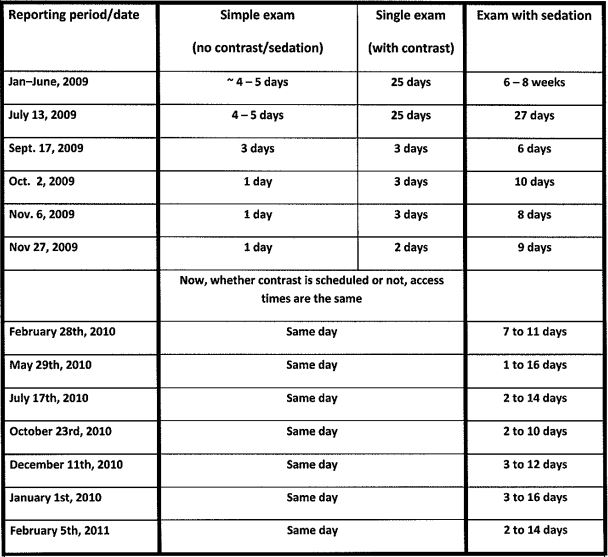
As is often the case with a level-loading solution, modifying the master schedule seemed counterintuitive, but it worked. More time was scheduled for each exam, a change that made it easier for the end-to-end process to absorb variability and remain level (on schedule). This eliminated the bottlenecks that were causing the long wait times for exams and results. In cycle-time terms, the “appointment-to-results” cycle shrunk drastically as the department got its scheduling process under control. As a result, more capacity opened, and this allowed an increase in throughput (appointments) without adding resources.
“Before the kaizen, the hospital was doing about 86 MRIs per week. Now, on average, we are doing 112,” Dulin said. “That is good news for our patients and the physicians who are waiting on the results of those tests. Instead of waiting 25 days for an uncomplicated exam, families can now schedule same-day appointments.” (See chart: Outpatient MRI Appointment Wait Times.)
The project significantly improved the hospital’s bottom line, with $1.2 million in additional revenue attributed to the better MRI scheduling.
It also earned ACH an honorary mention award at the International Quality and Productivity Center’s Lean Six Sigma & Process Improvement Summit in January, 2011. The award was in the category of “Best Process Improvement Project Under 90 Days,” with Akron Children’s competing against five other international companies and organizations that were selected as finalists.
Surgery: Greater Capacity, Higher Quality without $3.5 Million Expansion
Perhaps the most striking example of how lean processes will feed ACH’s efficient growth is the avoidance of spending $3.5 million to enlarge the sterile processing area within the surgery department. According to Mark Watson, president of the ACH Regional Network, surgeons were performing 12,000 operations a year, and the number of cases was increasing. (They performed 14,000 in 2010.) Sterilization technicians had a hard time keeping up, but expanding space and staff would have been a problem.
“Our surgery area is landlocked,” explained Watson, who first introduced the idea of lean process improvement to the hospital. “In order to give sterile processing more, I would have to take away from someone else. So we started really looking at what was going on in the operating room, and we started with our flash-sterilization rate.”
The team decided this was the most urgent need — a flash sterilization rate of 10 percent was not acceptable, Watson said. (Flash sterilization is the immediate and unscheduled sterilization of instruments that have been dropped or otherwise contaminated during the surgery processes. It is a quality problem that creates variability and waste.) They scheduled a kaizen focused on reducing flash sterilization. The resulting improvements not only reduced flash sterilization to 2 percent, but also opened all the capacity needed to add an additional 4,000 surgeries a year.
“It was amazing what happened in the week-long program,” Watson said. “We fixed flash sterilization, and increased the capacity of the operating room to 16,000 cases. We invested in one flat-screen TV, and we took down one wall. We have a sterile processing department that could handle all the work that was there and more without expanding one square foot.
“And now, we’ve done two capacity studies on surgery, and we are running at 64 percent. It will take 2.5 years, but we want to get to 85 percent efficiency, which would mean around $15 million in additional revenue in the same operating room with essentially the same people.”
Low-Tech Solutions Increase Customer Value
In addition to increasing the number of procedures, the hospital is focusing on patient value in the form of decreasing wait times and increasing accessibility to doctors and services. This supports the goal of being the No. 1 choice for Northeast Ohio parents.
Outpatient doctor visits was an obvious place to start. If there is any customer who is most deserving of getting more from service providers, it’s a parent with a sick child. Emotionally drained and frequently exhausted, such parents value predictability and kept promises. Less time spent at the doctor’s office means more time to take care of themselves and their families.
The doctors, nurses, and other employees at ACH’s Locust Pediatric Care Group know this. When deciding on a process improvement goal, their focus was reducing the amount of time that established sick patients spend in the clinic. By its nature, the clinic is an unpredictable place as patients stream in from the city of Akron and surrounding urban and rural communities. Many of the children are poor, recent immigrants, or in foster care. All of them have potentially complex social and medical needs, and all of them receive care regardless of ability to pay.
Through a series of kaizens and A3-based project planning and implementation, the Locust team identified and implemented a number of improvements that reduced patient in-clinic time from 70 minutes (2009) to 43 minutes (2011). Significant improvements included:
- Converting paper charts to electronic medical records, which helped to streamline the information flow.
- Implementing visual whiteboards that track patient flow during the appointment.
- Adding a team-wide “huddle” at the start of the day to prevent problems, such as scheduling issues.
- Eliminating triage rooms — where patients would be evaluated for priority of care — instead using mobile triage carts in the exam room.
The team is working on more definitive documentation, but early feedback is that customer value has increased.
“Office flow and access are the two biggest areas at Locust Peds where we can meet and exceed expectations from our patient families,” said Cindy Dormo, vice president for Pediatrics. “Now we’re measuring patient throughput and reviewing feedback from patients, which in the past has included complaints about long wait times, but is now turning favorable.”
Blue Belt Training Brings More People In
Dormo and other top-level executives said a key to the COE’s success is a focus on engaging all levels of the organization. Most recently, the COE team created a Blue Belt training program to focus on department and functional leaders, positions that would be considered “middle management” in a corporate setting. According to Dulin, the Blue Belt program is another example of how the COE program is directly supporting strategic growth goals.
“Our goal is to have this touch everyone. We then have everyone supporting the hospital’s goals, which then improves all of our major systems,” Dulin said.
Taking advantage of interest and enthusiasm generated by the MRI project’s success, the COE team chose the radiology department for the first Blue Belt training program. Every lead technologist, supervisor, manager, director, radiologist, the department chair and vice president participated.
Blue Belt participants learn how best to use the talents of their staff to streamline operations, improve the quality of care provided, and reduce variability and waste. Lessons focus on daily communication among staff members and leadership, learning how to track and improve daily metrics, and creation of standardized processes that stabilize patient flow.
The Blue Belt program is spreading to other departments. The plan is to begin with Dept. of Pediatrics employees, and then expand to surgical subspecialties, the Akron Children’s Heart Center, and Neurodevelopmental Sciences Center. In all at least 300 employees will have completed or been affected by Blue Belt training by the end of 2011.
Lessons Learned and a New Opportunity
Watson, the hospital executive who introduced continuous-improvement at ACH, identified these key factors as contributing to the COE’s early success:
Founding COE leaders: “After the decision was made to go with lean, I spent almost three months selecting people from our organization to help us on our lean journey,” he said.
Watson purposefully chose individuals who were successful, respected by their peers, and brought diverse backgrounds to the effort. These included a doctor with lean six sigma knowledge, a pharmacist who had just completed her Pharm.D., a medical technologist, a nurse, an M.B.A., and an administrator.

Watson also stressed the importance of having a practicing physician on the team. When Dr. David Chand joined ACH after working as a consultant, he dedicated 20% of his time to the COE and the rest to seeing patients. His role in the CEO has since expanded to about 90% of his time, but he will always see patients.
“When you are dealing with physicians, in order to be considered part of the club, you really need to have a stethoscope and see patients,” Watson said. “They like to interact with other physicians who are seeing patients. That’s just the way it is.”
Chand has been invited to work on improvement projects in many areas of the hospital and has become the go-to man for other doctors interested in learning more about the COE, some of whom are in the process of green-belt certification. His personal A3 projects have included removing non-value-add time from the residents’ patient-rounding process (daily in-person visits to patients).
Investing in education and training: Watson said an additional attribute that he looked for in team members was a quest for life-long learning.
After he assembled the team, Watson immediately sent them to a lean six sigma program at Johns Hopkins University, which included six weeks of learning over a four-month period of time (with project work done at ACH). The team then spent a week at Seattle Children’s Hospital to observe and learn from that CI program. In 2010, two team members received master’s degrees in operational efficiency and black belts from Ohio State University. Three others are now going through the course and will graduate in 2011.
Additionally, several department VPs have attended classes at Johns Hopkins and programs at Seattle Children’s Hospital.
“But we made a mistake,” Watson said. “When we started, we started with our front-line people working on projects with the A3 process. And we had very good engagement from the executive level, vice president and above. But what we left out was that middle manager level.
“Now the middle managers are really enjoying and learning with the Blue Belt program. The A3 process works much better now that we’ve covered the entire organization in terms of learning what we are doing. Our tagline is process improvement through people development.”
Accepting failures/celebrating success: Not every project will be successful, Watson said, “and if they are all successful, you are not taking enough risks.”
ACH’s ambition is being noticed and rewarded outside of its own facilities. This year, it was awarded a contract by a third Cleveland hospital, MetroHealth Systems, to provide pediatric care in cardiology, gastroenterology, cancer and blood disorders, and critical care.
“We are impressed by how fully Akron Children’s is integrated into the region, how well it has partnered with other hospitals, and its growth, having added 77 individuals to its medical staff in 2009,” said Margaret Stager, chair of the Dept. of Pediatrics at MetroHealth. Previously, UH pediatric specialists were contracted to provide the services.
Akron Children’s Hospital Center for Operations Excellence
A3 Program
- Started in January of 2009
- Eight-week Lean Six Sigma Training designed for the people who do the work on a daily basis
- Projects are done on A3 paper using the DMAIC (Define, Measure, Analyze, Improve, Control) methodology
- Meet weekly for two hours of class time and one hour of coaching
Green Belt Program
- 10 Green Belts certified through Johns Hopkins Center for Innovation in Quality Patient Care
- 20 Green Belt candidates working on certification through Akron Children’s Hospital’s Green Belt Training Program
- Candidates and projects selected by hospital leadership
- Ten days of training and project work spread out over five months using DMAIC methodology
- Tollgate session at the end of each DMAIC step
Kaizen Program
- Two-to-five-day rapid process improvement events
- Strategically driven by hospital leadership
- Multi-disciplined teams that cross over value streams
- Key stakeholders from the value streams work together to solve problems and implement solutions
Blue Belt Program
- Manager/Leader Lean Six Sigma training for departmental certification
- Basic understanding of Lean Six Sigma principles and tools: gemba walks, daily huddles, value stream maps
Related Information
Akron Children’s Hospital: As the largest pediatric healthcare provider in northeast Ohio with hospital campuses in Akron and the Mahoning Valley, the dedicated team at Akron Children’s Hospital promotes the well-being of children now and in the future. We perform more than 600,000 patient visits each year at more than 85 locations. Our specialists care for infants, children, teens, and adults treating a wide range of conditions from routine primary care to the most complicated injuries and illnesses.
Akron Children’s earned the Gold Seal of Approval from the Joint Commission, as well as Magnet Recognition Status for nursing excellence from the American Nursing Credentialing Center. We are a major teaching affiliate of Northeastern Ohio Universities Colleges of Medicine and Pharmacy, and offer a number of pediatric subspecialty fellowship training programs. Our Rebecca D. Considine Research Institute is committed to advancing the prevention and treatment of pediatric illnesses and supporting the education and training of research staff. For more information, visit www.akronchildrens.org.
- Read an interview with Bill Hopkins, Akron Children’s Hospital Board member, as part of the Lean Enterprise Institute’s executive series on lean leadership.
- Akron Children’s Hospital is a member of the Healthcare Value Network, a network healthcare organizations share their lean methods and experiences to accelerating each organization’s “lean journey. The Healthcare Value Network was created as a partnership between the ThedaCare Center for Healthcare Value and the Lean Enterprise Institute.
- The Lean Enterprise Institute (LEI) teaches many of the lean management and lean healthcare concepts described above through workshops, Lean Summits, books and workbooks, and on its web site.
- Join LEI’s Lean Community for lean management case studies, webinars, newsletters, thought-leading columns, and e-letters, and many other resources for starting and sustaining a lean transformation.
Lean Enterprise Institute, Inc. was founded in 1997 by management expert James P. Womack, Ph.D., as a nonprofit research, education, publishing, and conference company with a mission to advance lean thinking around the world. We teach courses, hold management seminars, write and publish books and workbooks, and organize public and private conferences. We use the surplus revenues from these activities to conduct research projects and support other lean initiatives such as the Lean Education Academic Network, the Lean Global Network and the Healthcare Value Leaders Network. Visit LEI at www.lean.org for more information.