In 2001, Massachusetts General Hospital (MGH) opened the Northeast Proton Therapy Center, a $50 million dollar facility for proton radiation therapy. The proton center is currently just one of three such clinical facilities in the U.S., and for many adults and children it is their best hope of beating cancer. Any bottlenecks or inefficiencies that delay patients from beginning and receiving proton treatment can have an adverse effect on outcome. Facing this compelling need to accommodate more patients through the center, MGH looked to lean. Rarely has improving a process been so important.
The Northeast Proton Therapy Center (NPTC) emerged from pioneering work at the Harvard Cyclotron Laboratory, Harvard University, where from 1961 to 2002 MGH physicians used 160 million electron volts (MeV) proton beams — positively charged subatomic particles — to treat disease. The new 44,000-square-foot, Boston-based NPTC began clinically treating patients in 2001 and includes three treatment rooms; immobilization, fabrication, and storage areas; mechanical, electrical, and vacuum shops; and treatment-planning facilities and offices.
“Proton therapy is a highly sophisticated component of radiation oncology,” describes Kathy Bruce, technical director for radiation oncology at MGH. “It uses a particle beam comprised of protons that are accelerated to a rapid pace, and once they hit tissue they have some special physical properties that are very beneficial in terms of radiation dosage to the area we want to treat vs. the area we want to protect. In many cases, tumors are adjacent to critical structures where the sensitivity of those structures limits the amount of dose we can give through conventional [radiation] means. But because of the physical property of the protons, we can do it differently and protect those structures.”
From the time NPTC opened its doors it sought to expand patient mix and volume, but while enhancements occurred, there continued to be pent-up demand for proton treatment. Last year 25 to 30 patients were treated per day, while the initial target for the center was 40 to 50 patients per day. “We had to look at the way were doing things to see how we could speed up the process without compromising the quality,” says Bruce.
While more patients with access to the proton beam can mean more opportunities to save lives, it’s not simply a matter of increasing throughput. Proton therapy is a complicated amalgam of medicine, physics, engineering, and compassion and involves treatment processes that few people will ever encounter and an incredible array of professions, processes, steps, and handoffs.
Dr. Jean Elrick, MGH senior vice president of administration, says there are more people and disciplines involved in the proton center’s therapeutic identification, planning, and implementation processes than in any other facet of care at MGH. The process includes engineers, physicists, nurses, therapists, doctors, residents and fellows on teaching missions, anesthesiologists for children, and a machine shop — all in a new facility working with new technology. “And that’s just the clinical part, let alone all of the surrounding pieces of support that go into that clinical process, which makes it all the better place for lean because of how quickly on a relative basis that very complex, multiperson, multifactorial process could be so clearly laid out.”
The Proton Therapy Process
NPTC’s 230 MeV proton beam originates at a cyclotron, a machine that accelerates particles to their multimillion electron-volt energy level. The beam is steered with huge magnets through concrete tunnels the length of a football field into one of three patient-treating areas — two gantries and one stationary treatment area. The beam peels off the main line and serves one treatment area at a time.
The gantries are massive 110-ton spherical structures that slowly rotate to any 360-degree angle within one millimeter of accuracy around a stationery patient. Patients, fitted with specially designed masks and molds, are positioned to within one-half centimeter of their calculated treatment position. The proton beam is targeted from any angle into three dimensions to match the shape of a patient’s tumor. Apertures and compensators are incorporated between the beam and patient, which direct and constrain the protons to the desired 3D areas; one patient may require multiple devices.
The beam-on time for a patient typically is between one minute and two minutes per field (the targeting of the beam from a given direction), and a patient may require from one to seven fields during their treatment session, says Susan Michaud, RTT, assistant chief radiation therapist of radiation oncology and supervisor at NPTC. Some complicated pediatric cases take more than one hour to set up and treat.
Children also require general anesthesia to receive the proton therapy in order to remain immobile. Each room is set up with an anesthesia cart and backup systems, and an anesthesia team works on every single child case using a fast-acting drug, which knocks them out and brings them back quickly after treatment. “For some of these children,” says Dr. Elrick, “this is the only therapy available to them, ever.”
For many patients that come to NPTC, “this is their last hope,” says Michaud. The center offers treatment options that go beyond what can be accomplished with a conventional photon beam, and “that’s why we pick them to get protons.”
When a patient or referring physician requests treatment from NPTC, an “intake” process begins to identify the appropriate candidates via preliminary diagnostics. After this stage, NPTC clinicians and physicists conduct “proton rounds” — a thorough assessment of a patient’s need for protons and the potential benefits of proton radiation to the patient vs. other forms of care.
For patients selected to receive protons, a three-dimensional reconstruction of the patient’s tumor relative to surrounding body structures is made and a reproducible treatment position established (an immobilization device is created for each patient allowing them to replicate their position for each treatment session, typically 30 to 35 sessions per patient over several weeks). Once a patient’s immobile position is defined, a computed tomography (CT) scan is taken, creating multiple image slices of the body at two- to three-millimeter intervals for treatment planning. The physician then electronically draws the tumor and surrounding tissue for each image slice, and, along with dosimetrists, who calculate radiation dosage, plots out a computer plan for how protons enter the patient and attack the tumor. This plan is downloaded to milling machines in the NPTC machine shop, which manufactures the apertures and filters.
The Lean Approach
Patient time under the proton beam is minutes and offers no opportunity for time-savings. But the preparation time prior to patients receiving their therapy, the intake process to identify and schedule proton patients, and the treatment planning processes were ripe for improvement and could lead to greater patient volumes.
NPTC’s need to increase capacity also coincided with a multipronged strategic plan at MGH, instituted under president Peter Slavin, which focused on process improvements and cost-savings hospitalwide. Dr. Elrick, the chair for the process-improvement strategic planning committee, had reviewed various improvement approaches, including lean, and attended a presentation by the Lean Enterprise Institute (LEI). She selected the proton center as a lean pilot project and “volunteered” Nancy Corbett, senior administrative director for the radiation oncology department to set lean in motion; Carey Palmquist, administrative director of practice operations, and Kathy Bruce supported Corbett.
Helen Zak, COO of LEI, and Guy Parsons, an LEI faculty member, reviewed the NPTC operations and its capacity challenges. They presented an approach of how lean principles could jumpstart improvements in the center via three days of workshops that involved a scoping session with leadership and value-stream mapping and action-plan sessions by a lean team. The leadership of the NPTC (Dr. Thomas DeLaney, medical director; Dr. Hanne Kooy, associate director and manager of radiation physics at the NPTC; and Dr. Jacob Flanz, technical director of the center) bought into the lean plan, says Corbett, once they were convinced that lean could “subtract” things that got in their way of providing the best possible care for patients.
Parsons was able to impress upon Dr. Elrick and NPTC staff the means to improve processes without touching and tampering with the caregiving component. He assured them that the initiative would “not talk about appropriateness of care. We don’t know about it. It’s everything else.” Everything else in lean terminology was the “waste” in the processes, the issues and obstacles that frustrated NPTC staff and prevented them from administering therapy in the most efficient and highest-quality manner.
The LEI approach, adds Dr. Elrick, also was dissimilar from the armies of well-dressed consultants who conduct interviews, distribute reports, offer copious recommendations, and link efforts to information technologies or long-term engagements. “I’ve been doing change management for 12 years; it has to come from within. This has to be us, not you.”
“We do the best we can do in three days, as opposed to other organizations that would view this as an opportunity to add on more and more days,” says Zak. “The key points we emphasized with [NPTC] is that they need to take it from here, and do the detailed implementation themselves, that they’re the ones that own the current and the new process, not us.”
While the overarching goal was to increase the number of patients treated through NPTC, another goal was to have proof of concept for everyone else in the hospital, and thus link it to MGH’s strategic plan, says Dr. Elrick. “The more successful [the proton center] could be, the better it would be for everybody else.” Because of that, in addition to people charged with handling the proton center transformation, there also were “observers” from other departments involved in the lean workshops.
“One of the principles that I hoped we could establish was that this is a learning institution. We want people to be there understanding that it’s not the specifics that are brought back, but how you do things and how you apply lean,” says Dr. Elrick. “There was someone there from the department of radiology and the department of pathology, and we’ve subsequently done an engagement with pathology that has been tremendously successful.”
Lean Kickoff
The lean initiative kicked off in September 2004 with the scoping session during which NPTC leadership identified what could and should be goals for the effort and who should be involved in the subsequent two days of value-stream mapping and action planning. “We didn’t pick people that would be immediately agreeable,” says Bruce. “We picked people who would be key to the success going forward, who we knew would be difficult to persuade, who really owned it. Every discipline was represented.”
“It was not optional to come for part of the day if you were on the proton center team,” adds Corbett. “It was two days, beepers off, no answering pages. Participants, including physicians, had to have someone cover them for the full two-day commitment.”
For two days, a 15-member team of physicians and clinical and non-clinical staff drew a current-state map of the process, developed future-state maps, and set action steps and responsibilities that would move NPTC from the current state into the future.
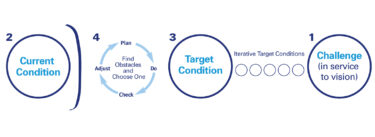
Current-State Maps
In drawing a current-state map, the team laid out in detail the processes involved with proton therapy, from the intake process and proton rounds through treatment and to post-treatment. Any issues related to first-time quality, waste, waiting, flow, etc. were then posted on the map using a process Parson describes as “affinity gathering” — the team put sticky notes on their wall-sized map wherever issues existed, and then grouped the issues into bundles or themes. “They finish up the day with a current-state map and clear picture of what’s broken,” says Parsons.
“I think one of the things that LEI learned about the proton center is that, although [LEI] had done some work in healthcare before, they had not done anything as complex as radiation therapy,” says Corbett. “They underestimated the complexity of their mapping in this.” She notes that NPTC staff also were surprised by the complexity, and at first would challenge the processes described by their own map — “Wait a minute, that’s not how it really works.”
LEI’s Zak says mapping was more complicated than they or the NPTC team realized, but “that’s typical, not only in healthcare but every other industry. People think they know what the process is. That’s one of the huge benefits of value-stream mapping — it really highlights what the real process is.”
To recognize the disconnect that can exist between the belief of what’s happening and the reality of the current state is a humbling experience, says Bruce. When developing the current state picture there was repeated input and feedback by the entire team, she adds, often with one member correcting another’s interpretation of the process. Ultimately, though, the team came away with a collective understanding of the entire process.
“The big revelation to them was the fundamental difference between the time that everyone would agree was necessary and valuable to the patient journey compared to the total time,” says Parsons. “That was probably No. 1. The second was a real ‘aha’ about first-time quality, which is a measure we use to look at every step and if, when you sit down to do that step, you have everything you need so that you can do it right the first time. First-time quality doesn’t say anything about what you complete; the quality of what they completed was wonderful. The issue was how much thrashing, scrap, rework, and hunting is required in order to deliver that perfect product out of your individual step.”
Future-State Maps
Development of the future-state map focused on how to build a process vision using a lean lens. Parson says when defining this future state and the changes to come, the team was forced to take a full view of the value stream, not just worrying about how the changes would impact their own work and actions or their own levels of efficiency.
“Someone who may have been reluctant to change or not motivated to change, now understands what he or she does and how that behavior impacts someone four steps down the line or four steps before it gets to them,” says Corbett. “Whereas if you ask someone to change for the sake of change, or some consultant comes in and says you ought to change, it’s a much harder sell. It’s not sustainable.”
The NPTC group was split into two teams, with one developing a high-level map that encompassed the entire patient journey, from the time they tried to schedule an appointment until they were done with their course of treatment. The second group mapped the narrow part of the process of when a patient is being readied for treatment, treated, and then released from that proton-treatment suite.
Again, the focus of future-state improvements had to do with time and activities external to the moment of clinical caregiving. Parson says, “The actual care-giving moment, the things everyone would agree were valuable and medically important, those things can be left alone. From a time perspective, they represent so little of the overall time through the system.” In healthcare and with physicians, value-stream mapping and the lean approach to waste elimination help to alleviate any concerns of intrusion into the doctor-patient relationship. “By focusing almost exclusively on when nothing is happening or when we’re searching or doing something that everyone would agree is not valuable, the physician starts to get comfortable that we’re not gunning for the way they deliver care.”
Action Steps and Action
After identifying how the processes could work better via the future-state maps, the team established 15 steps as part of its action plan and assigned a captain to each step (all but four action steps had been completed in early June).
The scoping session also had established signoff procedures for the leadership committee for changes that would emerge during this phase. First, leadership reviewed and voiced support for the general direction of the future-state maps, and, second, they backed the individual action items as changes they could and would support, says Parsons.
As steps were undertaken and achieved, progress was communicated regularly to NPTC and other departments through town meetings so that “everyone knew what was going on at the proton center and why,” says Corbett. The sessions were extremely well-attended, and the message of improvement was obvious. “It was concrete, measurable, real, meaningful. It wasn’t buzz-wordy. Change had taken place, and the results were measurable.”
Lean Improvements
Looking back at the lean sessions, Dr. Paul Busse, a team member and clinical director of the department of radiation oncology, says, “The interesting part, at least for me, has been the perception of everyone that works at NPTC. They collectively feel there was a benefit. That’s a little unusual because, in the medical industry, we tend to have a jaded
view of process improvement. To have physicians embrace it, as well as everyone else, is an unusual scenario, but this group did just that. Collectively we were part of the process, and collectively we reaped the benefit. Once we identified specific problems and then broke them down into their different elements, we were fortunate enough to see together how things improved.”
Among the achievements to date from the NPTC lean team are:
Accelerating Proton Rounds
An effort led by Dr. DeLaney improved proton rounds, the process by which patients are selected to receive proton treatment. Changes involved defining a class of patient that should bypass rounds and revising how rounds are conducted.
Proton rounds are conducted once a week. If a physician missed the weekly opportunity to review materials, it could be another week before a patient was accepted and four to six weeks before the patient could begin treatment. “If someone has a very indolent disease process, that’s OK. If they don’t, it’s not,” says Dr. Busse. “This gives us a more appropriate vehicle to get people into the system in a timely fashion. We really shouldn’t be wasting everyone’s time in proton rounds discussing cases where it is a fait de complete that it be acceptable. One of the things we discussed with [Dr. DeLaney] is a set of criteria for the patients we knew we would treat, for which we would always say, ‘Yes.’”
Because of improvements to proton rounds, the time from when a physician requests that a patient be eligible for proton treatment to the start date for treatment planning has been reduced from five days to three days.
“A key to the success,” says Parsons, “is that improvements were done with four physicians in the workshop … working together with everybody. In medical environments, there is often a wall between the different functions, and certainly between the medical and the allied staff. The fact that they were willing to get in the room and push through hard issues to create a common vision for the future helped make it stick.”
Improving acquisition of patient information
NPTC receives many requests from patients, their relatives, or their physicians for treatment, and these individuals communicate the need for proton therapy. This front-end of the intake process was originally assessed by the lean team as having between 0% and 10% first-time quality, meaning that, after the first encounter between a potential proton patient and NPTC, rarely did the center have sufficient information by which to determine need and move forward.
“So many different people, whether it was the patient, a patient’s friend, or the patient’s referring physician would call and not know what questions to ask or what facts to have with them in order to get on the docket,” relays Parsons. NPTC staff would repeatedly follow up with prospective patients or their physicians, which led to “telephone tag” and delays. “One of the countermeasures was to develop a clear checklist of things that people need to know before they try to present themselves.”
Standardizing Treatment Planning
Treatment planning is a complicated process where an attending physician develops and reviews a patient’s proton dosage volumes and targets, completes an analysis of a treatment plan, and then approves the approach. Lean action steps have emphasized clear and consistent documentation of the process so it’s quickly understood by everyone that each step has been completed, thus allowing treatment to proceed (machining devices, scheduling treatment, etc.). In addition, visualization methods have been used to encourage physicians to finalize the process within a matter of days.
“That was a very limiting step for us,” notes Dr. Busse. “Not everyone was doing it in a similar way, and sometimes there were revisions afterward that led to a duplication of effort.”
Standardization of forms and improvement to the process has made a significant difference. Dr. Busse says, “I can tell patients, look them straight in the eye, and say, ‘You’re going to start in three weeks,’ as opposed to getting phone calls from a patient’s referring physician asking, ‘Why hasn’t this patient started? What’s the hang-up?’”
Availability for Pediatric Patients
The team established an action item to increase the number of “anesthesia slots,” treatment times available to children. “If there is ever a sense of urgency around getting a potential patient to treatment as soon as possible, it always has to do with these children,” says Bruce. “We worked with the anesthesiology department and came to some agreements on increasing the number of hours that they could be committed to [NPTC] patients every day, basically doubling their availability. Double the time means double the number of kids under anesthesia.”
Decreased Patient Time in the Therapy Suite
When discussing the processes that take place in and around the treatment suites, Parson says, the team followed an analogy to a NASCAR pit crew — while the car is on the track, the pit crew is busy working, preparing for the next opportunity when the car enters pit row. In NPTC’s case, the team is preparing for the next patient while the suite is in use.
“The bulk of the real improvements came out of anticipating and preparing in a higher quality way than they had originally done, which previously was putting the patient in the room and then starting to search for all the things they need to deliver treatment,” says Parsons. The team established methods to make it easier to find, identify, and handle patients’ immobilization devices and apertures, and as a result reduced the time to prepare patients for treatment — and consequently moved patients more quickly through the suite, to the benefit of patients and without impacting quality.
NPTC also changed the way patient slots are scheduled, no longer reserving precise times for patients; previously, if a patient didn’t show, a valuable slot might go unused. “Turnover is faster and the next available person takes the next available slot,” says Dr. Busse. While the schedule may “bulge” when patients are dropped into the schedule because they absolutely must get immediate treatment, NPTC has developed methods to flex with the bulges to accommodate all patients, such as extending the working day.
Digital Imaging
The Department of Radiation Oncology is introducing a new electronic digital imaging system, electronic scheduling, and database management of images. While not solely driven by the lean initiative, the implementation of these new technologies will draw on lean principles to obtain maximum benefit for all users.
“We have a whole different set of handoffs and whole different workflow than we had before,” says Bruce. “So we’ve selected that as an area of concentration in order to roll out this new technology in a way that isn’t frustrating but, in fact, beneficial in terms of efficiencies, etc. We want to develop that ideal state as to how we’ll ship images around the department.”
This new desktop-to-desktop flow process should begin by the end of summer and will eliminate large amounts of time, errors, transportation, and handoffs associated with conventional x-ray film (e.g., darkrooms, film handling, inner-hospital mail service). Though still complex, it should be much simpler than the previous process.
Continuous, Measured Improvement
On their current-state map, the lean team had defined measures for first-time quality, wait time, and work time, says Palmquist. They used these as the starting point for the future-state map and established goals toward improving each measure as much as possible. “Not to be perfect, but to make them better.”
Establishing measures wasn’t always easy or obvious. For example, the intake time, from when a patient requests treatment to when they begin treatment, is now a tangible figure that can be improved. As such, the lean team projected how the key hiring of an intake manager can reduce the total intake time. Initially, Palmquist notes, there were no measures for the intake process, and they believed it wasn’t even possible to measure the process.
The work of the lean team has increased capacity at NPTC to on average 45 persons per day, meaning 10 or more people daily now have access to the proton beam than they did just months ago. And NPTC is doing that with the same number of people as when the transformation began, meaning unit cost per therapy has dropped. “This is not a long period of time over which we’ve done several things and had measurable outcomes,” says Dr. Elrick.
But no one is complacent. “This exercise is not about getting perfect, it’s about getting better,” says Corbett. “It’s about making changes where we can. Don’t expect we’re going to get to that ideal state at the end of the process. We want to make chronic improvements through our whole lifetime in delivering care. I think that was an important expectation to set early — don’t think this is going to be absolutely right.”
Getting better at NPTC has been driven by setting realistic targets. The timing of action plans and outcomes — “short-term, tangible, and attainable” — was important for people accepting lean, says Palmquist. “They weren’t things that we were going to reach in a year. The action plans we came out of the room with were things we could do in 90 to 120 days. And that made it comfortable for people, and it made it nice for people who were advocating for this, who could say, ‘We can see change.’ Those little things will have a large impact in a short term.”
“The action plans are not intended to be much beyond 90 days,” adds Parsons. “If we go much further out, people start imagining new IT systems and other big-think answers instead of answers in the spirit of continuous improvement. So we try to keep that planning horizon short.” He says MGH probably achieved all the benefits of the workshop six months down the road, “but they were getting better within weeks after the workshop and just continued to make improvements upon improvements once they got momentum.”
The structure of the workshops supported a lean tenet that encourages organizations to fix the process, and then invest in the process if necessary. Prior to the lean effort, NPTC staff had requested as many as 10 new hires as the solution for growing capacity. Corbett was in the process of assessing this HR need when the lean project emerged. She believes NPTC now is approaching capacity and may extend hours to grow volume, which will likely require additional staff. “Which is where we started, except that we’ve tightened up and improved our throughput, and we’re continuing the lean process. Now we’re making smarter decisions about who we need and where we need them.”
While lean is not capital intensive, notes Corbett, there were expenditures necessary to achieve goals — but now there is lean rationale for spending. For example, the team set an action step to hire an intake manager; when on staff, this person will coordinate the steps for bringing new patients into the therapy process. Also based on lean teamwork, NPTC installed a paging and audio system that reached to the second-floor of the building (where most staff are located). But, Bruce points out, this improvement scenario is quite different from previously when the only answer offered to grow volume was to add people.
Today, Corbett, Bruce, and Palmquist regularly revisit processes, seeing if improvements are sustained and looking for additional improvement opportunities, and they’re carrying the lean message to other parts of MGH. Dr. Elrick also conducts events off the MGH campus and has done presentations for the MGH general executive committee, which is comprised of the administrative and clinical leaders of Massachusetts General Hospital.
Expanding Lean
Now that lean has proven its merit at NPTC, it can likewise be applied to other oncology departments and throughout the hospital network, reasons Dr. Busse. We have 40 patients that go through the proton center on a daily basis, and 180 to 200 patients that go through the main department. So if gains are being realized at the NPTC, imagine the potential impact.”
Like the patchwork addition of buildings and wings to most hospital campuses through the years and decades, many hospital processes have similarly evolved, says Dr. Busse. “We need to break these out and find out where the inefficiencies are.” Adds Dr. Elrick, “Every one of those changes had good rationale, but they just add up over days, weeks, months, years, decades, centuries, until one minute you say, ‘Whatever were you thinking?’”
LEI’s Zak agrees that the entire healthcare industry, not just lean pioneer MGH, is ripe for lean improvements. “Healthcare has a lot of waste, and taking a look at what healthcare systems do through a different lens shows a huge opportunity. And lean focuses on that nonvalue added stuff; it doesn’t focus on the clinical portion. We leave that up to the experts.” She says that lean pioneers in healthcare start their transformations in different locations, some on nonclinical processes that touch everyone (admissions and discharge) and others where there is great need and great return (operating rooms and emergency departments). “It gets down to each healthcare system asking, ‘Where are we most not meeting the customers’ needs?’ and trying to start there.”
Dr. Elrick says the proton center was “a good place to start — good leadership, talented people, and compelling issues. It was the perfect environment. That’s how it started out, and, from my view, it’s been wonderfully successful.”
Just as the medical and scientific breakthroughs at NPTC will benefit new proton centers around the country that will come online, so, too, will its process improvements provide much-needed benchmarks. “This facility has been the first for many things, and from our development other centers are going to benefit,” says Michaud.
Closer to NPTC, other MGH departments and personnel, such as pathology, are being convinced of the lean approach. Just as it was impressed upon NPTC staff, Bruce says she is citing the subtraction of nonvalue from the process and the “easy metrics of wait time, work time, and first-time quality. You don’t have to have a Harvard MBA to understand those things. It’s so simple to get these points across. It doesn’t require great managerial insight. You don’t have to be a multiple author of management textbooks to get it.”
The simplicity of lean has always been core to the methodology’s successes, dating back to its origins out of Toyota that worked from principles derived by peasant farmers — average people operating an excellent process. NPTC certainly has upped the ante, though, relying on extraordinarily talented people across a spectrum of challenging professions working to improve a complex, life-saving process. And, most importantly, they’re succeeding, and people are living longer because of it.
For more information
Massachusetts General Hospital’s Northeast Proton Therapy Center: Massachusetts General Hospital is a founding member of the Partners HealthCare System, an integrated healthcare delivery system comprising two academic medical centers, specialty and community hospitals, a network of physician groups, and non-acute and home health services.