Waiting is an activity that few find rewarding or of value; it’s simply a waste of time that reduces anyone’s level of satisfaction. Yet, somehow, healthcare and waiting often are synonymous. The Clearview Cancer Institute in Huntsville, AL, is a dramatic exception. Physicians and staff have tirelessly reengineered the institute’s processes and patient flow to eliminate as much waiting and waste as possible. They have implemented a range of healthcare process innovations that make the new facility atypical, and, in doing so, improved their ability and capacity to serve cancer patients and, most important, they improved the patient experience.
The new $29 million Clearview Cancer Institute (CCI) began seeing oncology patients in October 2006, having moved from a facility where founder Dr. Marshall Schreeder and his colleagues had begun reengineering the way they served patients. Dr. Schreeder says the level of “service” the institute can offer patients improves the ability to treat them effectively and efficiently and is at the core of healthcare. “I think the recognition that healthcare is a service industry is out there. I think most people who want to improve what they’re doing recognize that. I don’t think I’m unique in that regard.”
But Dr. Schreeder is unique in another regard. While board certified in internal medicine, medical oncology and hematology, he says he is “plagued by an industrial systems engineering background” (he graduated from Georgia Institute of Technology with an undergraduate degree in industrial and systems engineering): “It kind of hurts to see something that’s not operating right. Our competition is our own inefficiencies. If we’re going to do the best we can do, we have to pay attention to our processes. We have to pay attention to outcomes. There is no reason to talk about outcomes unless you talk about processes.
“Healthcare has to take a look at what it’s doing with the same tools as industry,” he adds. That belief led him and CCI to enlist lean assistance from a small team lead by Maruf Rahman, director, process improvements initiatives, Office for Economic Development, The University of Alabama in Huntsville.
Improving the ability and capacity to treat cancer patients is important given the number of persons afflicted with cancer and the relative efficacy of treatment. The American Cancer Society predicts that 1.44 million people will be diagnosed with cancer in 2007 and 560,000 will die of the disease. The absolute numbers are disheartening, but the Society reports that for the most recent reporting period (2003 to 2004), cancer deaths dropped by 3,014, and the death rates from all cancers (indexed by population totals) decreased from 1990/1991 to 2003 by 16.3 percent among men and 8.5 percent among women.
CCI is one of only a handful of oncology treatment facilities serving an area of approximately 3 million persons, so capacity is a concern. “[Dr. Schreeder] was seeing a serious growth in cancer patients at his existing facility,” says Rahman. “He could see that his existing facility would not be able to handle that load.” Rahman’s team and institute staff — led by Dr. Schreeder and administrator Lee Horton — assessed the previous facility and how improvements could be made there, and they also compiled recommendations for improving patient flow for a new facility that would be built, incorporating their learnings into facility design as well as the processes that would take place at CCI.
Patient Flow
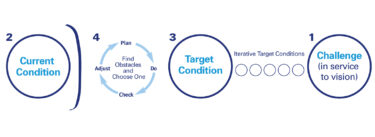
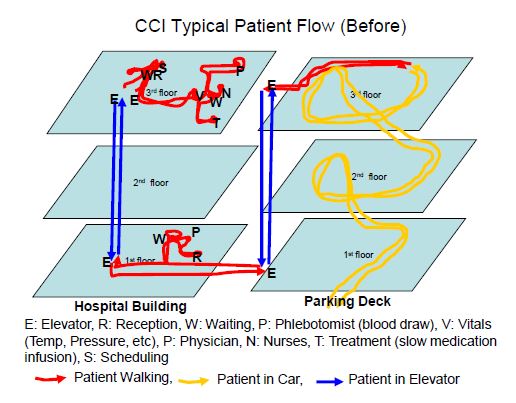
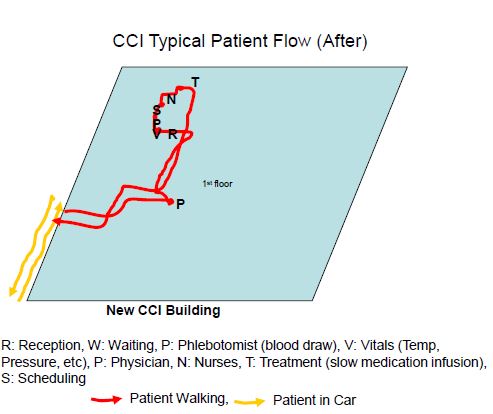
CCI’s improvement strategy was never termed “lean,” yet it did begin with the core lean concept of value-stream mapping. Staff mapped how patients navigated through the previous facility and its services; where patients waited and why; and how physician and staff time and energy were spent moving about and treating patients. Horton says, “We looked at everything as linear. We plotted the steps of the patients and designed the building that way.” In doing so, the new facility incorporates patient flow patterns not possible in the previous facility.
For patients, the changes are recognizable even before setting foot inside the new institute. An expansive, covered dropoff lane accommodates 15 cars, and a curbless lane ensures easy access for the institute’s many wheelchair-bound patients. In the previous facility, most patients would have entered from an adjacent parking deck and navigated through stairways and elevators — the new entrance cuts up to 20 minutes from their visit. “They just open the door and come right in. Nothing to it,” says Dr. Schreeder.
Once inside, patients follow a carefully choreographed path that flows them — in many cases unconventionally — through the facility. For chemotherapy patients receiving slow-medication infusion (the majority of the institute’s patients), the path takes them from lab work through their physician exam, scheduling, chemotherapy treatment, and then out the door (see Patient Flow diagrams below).
Reducing Waiting
Lab work is where blood is drawn and analyzed to ensure patients are able to receive treatment, and nearly all CCI patients (98 percent) require lab work. A process improvement implemented in the previous facility was to have patients go immediately for lab work, and, in the new facility, that concept was extended through design and the placement of the lab at the front entrance. While getting their lab work, patients also are registered into the institute; wherever the first point of contact is for a patient, they’re automatically registered and their flow set in motion.
“Lab is a rate-limiting factor,” says Horton. “The doctor can’t make any decisions until he has lab results.” The lab work is completed while the patient moves to a reception area where they’re greeted and vital signs checked prior to entering a “pod” (a cluster of exam rooms, a dictation room, and physician support services) to see their physician. This is unlike many healthcare facilities where patients wait to see their physician, only to be sent to the lab and then back to the doctor where they wait (again) for the lab work to arrive.
“Certainly by the time they’re in the [exam] room, the laboratories are already run and available,” says Dr. Schreeder. “We’ve overlapped those processes, and that’s helped.”
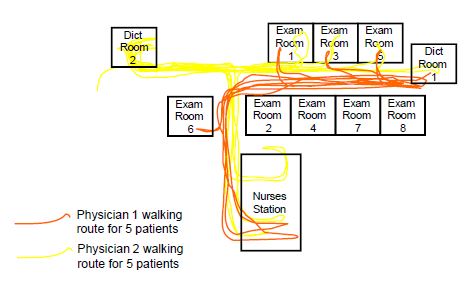
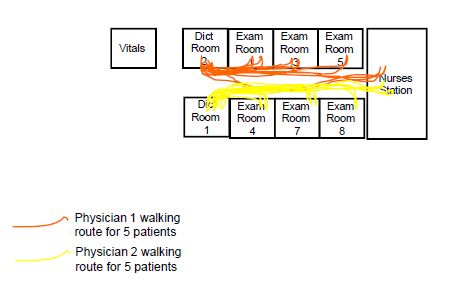
Two physicians each use four pods (eight physicians total), and the layout of every pod is standardized. Horton says, “Every piece of equipment is exactly the same so that we can move our staff back and forth, and medical records and central [personnel] will know where things are.” Exam rooms previously were arranged in rows down a hall, and whatever room was open is where a patient would be placed and their physician instructed to go. The layout had physicians moving from room to room, often from one end of the hall to the other and then back again as they examined patients, gave dictation, or worked with a physician assistant. The pods position exam rooms in a pseudo-cellular manner so that they are adjacent to dictation areas and the physician assistants (see Pod Flow diagrams below).
Two Physician Non-Cellular Layout (Before)
Two Physician Cellular Layout (Current)
A real-time central system is being implemented to collect and disseminate patient information to physicians and staff as the patient moves through the institute. For example, physicians will access patient files electronically in their pods via Blackberry handheld devices. Most of the electronic information flow is in place, except patient charts, which are still currently paper-based.
Once at the pod, the physician examines the patient, prepares their chemotherapy order, readies the patient to leave the exam room, and then begins dictation. The patient proceeds to scheduling, and a non-physician employee takes the patient chart and the chemotherapy order to admixture (a process point that Dr. Schreeder describes as still “a weak link in the system” that electronic ordering will fix, enabling first-in, first-out of orders and further reducing patient time at CCI).
Quality Checks
The chemotherapy admixture is prepared in a biologically safe hood room according to the physician’s order, and then reconciled with the order and with billing — a quality control check to help ensure that the drug ordered was indeed the drug given and then subsequently billed appropriately. The institute is planning to photograph and log every drug-delivery syringe alongside the drug’s barcode. This real-time electronic check — and record of the check — will enable a nurse administering the chemotherapy to see that the two components match. Currently, and as in most oncology centers, the reconciliation of drug and syringe is performed manually treatment by treatment, with no historical record that the check was made.
Meanwhile, as the chemotherapy is being mixed, the patient has moved from the exam room and to the scheduling department. “We found two time-consuming things that keepthe patients here,” says Horton. “One was mixing their chemo and [the second was] scheduling [their next visit]. So we plopped scheduling in between the physician visit and chemo, and they’re making their schedule while their chemo is being prepared.” If a patient doesn’t need chemotherapy, the location of scheduling services has been placed at the main exit hall, enabling such patients to quickly and easily leave without renavigating the patient flow.
Each physician has their own scheduler, a person who is familiar with the physician and can read their handwriting and understands their treatment habits. Horton notes that a consistent scheduler is better for the patients as well because they see the same person each visit, someone who’s familiar with their personal scheduling preferences and needs. Similarly, each physician has a primary nurse they work with, and nurses are assigned to a specific area so they get to know the patients (although they “float” as patient demand requires). From scheduling, patients move to the chemotherapy treatment area.
The airy treatment area is about three times larger than was provided in the previous facility, says Dr. Schreeder, with heated reclining chairs (fluids going into patients can feel cold compared to body temperature) and large windows that look out on to ponds and fountains. Artworks from regional artists adorn the treatment room and appear throughout CCI; the pieces, selected by Dr. Schreeder and staff, help to brighten a difficult patient experience. A patient’s time receiving chemotherapy can vary from minutes to hours, depending on the drugs administered and the cancer. Similarly, the frequency of treatment cycles can be weekly to monthly, and treatment can last from months to as long as the patient can tolerate the chemotherapy.
No “Hunting”
Next to each of the 60 standardized treatment stations is a portable cart and shelving that contains everything a nurse needs to administer the chemotherapy. Many items that were previously shared among stations, such as thermometers or blood-pressure testers, are now in ample supply at each station. That, as well as standardization, helps reduce any waiting caused by nurses searching for tools. Color-coding by physician, which begins in the exam rooms, extends into the treatment area; a whiteboard helps nurses identify specifically who’s occupying a treatment station and cuts down the time that nurses “hunt” for patients. The whiteboards identify patients by their physician and the treatment station at which they can be found.
The chemotherapy treatment area also is adjacent to the main exit hallway. Once the treatment is complete, “They’ve already checked out. They already have their schedule. They don’t have to stand in any other queue or checkout,” says Dr. Schreeder. “The place is designed with patient flow in mind, and I’d say it’s been very successful.”
Patients who don’t match the typical chemotherapy-patient flow as described above, such as those needing a “short infusion” or just a shot, follow a shortened route that prevents them from queuing up with everyone else. The institute opened a coumadin clinic in January, and a similar flow strategy will enable those patients to come in and avoid the general mix and queues of the chemotherapy patients.
CCI Keys and Key Results
Critical to the improvements at the Clearview Cancer Institute has been an understanding among staff and across departments that what anyone does and how they do it impacts staff in other departments and, ultimately, the patient flow. Horton says CCI now has cross-functional committees in which all departments — e.g., lab, nursing, the business office — are represented, reducing the likelihood for one department to make a unilateral decision. “Instead of creating a rule and a problem that ricochets down, now we look at how it affects every process all the way down,” says Horton. “It hasn’t been that easy, and we recently created a core management team of two of our most experienced nurses who are shepherding that.”
Another core piece of the improvements across the institute — and core to lean — is standardization. Dr. Schreeder and Horton see standardization as a means to reduce variation, and less variation means less likelihood of error and improved quality. Often this practice of deploying standardization derails improvement efforts in many industries and organizations because there is a sense that creativity or personal freedoms are being reduced, when, in fact, standardization establishes an efficient model for the routine that then allows creative, value-adding time to expand.
“The doctors have been amazingly flexible and willing to change,” says Horton. “The more variation there is the more there is room for error, so we are going to standardized everything. [Physicians] have agreed to standardized antibiotics. They’ve agreed on standardized antiemetics. They’ve agreed that this is our protocol. … We’ve really looked at how we can streamline the process.”
There has been significant growth in the variety of drugs available to physicians in recent years, notes Horton. From the multitude of drugs, physicians at the institute have standardized down to a smaller set of antibiotics that still affords them the flexibility they need. This facet of CCI change is unlike many lean healthcare implementations where the treatment component is never touched — i.e., remove waste anywhere but don’t interfere with the physician/patient moment. “It really has touched the patient component because of the standardization of orders, the standardization of care,” she says.
The CCI transformation has had moments of resistance — “Oh, we’re fine, we’re just like everybody else,” Horton recalls hearing. But Dr. Schreeder and Horton are not like everybody else. “We think we can always be better,” she says. “It would drive him crazy that we were constantly looking for charts, looking for people. … If you go to any community oncology clinic, it was the way we were. Nowhere you visited was it any different.”
Happier Patients
The differences at CCI now are striking: Horton says that 45 minutes were removed when the lab work was given priority and moved to the first floor in the previous facility. (The new facility has three floors, but research, administration, and office rentals occupy the second and third floors.) The concurrency of scheduling with chemotherapy admixturehas helped cut another 20 minutes from the process. A faster, superspinning centrifuge for lab chemistry, which used to take 30 to 45 minutes for a complete metabolic profile, takes about 15 minutes to complete and saves another 15 minutes. The dropoff lane is an additional 20-minute reduction for patients.
“We’ve easily taken an hour if not an hour and half off the typical day for them,” says Dr. Schreeder. “It seems as though the work has been cut in half. I thought for a while, „Where did everybody go?’” Both Dr. Schreeder and Horton note that while patient volume is the same or higher, the facility is often winding down by 5 p.m. — previously patients would have been waiting into the evening to receive treatment due to a day full of backups, delays, and waiting.
“We have been able to handle about a 45% increase in patient load in two years, and we have not added any medical records staff,” says Horton. “We have added more nurses for good reason — patients are living a lot longer and they’re coming back for multiple treatments. Every bit of money that we’ve spent we’ve gotten back in less personnel costs and, I think, less turnover, too.”
An additional half hour of patient time at CCI should be trimmed once the central communications system is fully in place, notes Dr. Schreeder. He also plans to “quantitate workflows” and conduct systematic optimizations that could result in more timesavings (i.e., now that the overall patient flow has been improved, incremental improvements can be targeted within functions/activities). But for him the ultimate measure of system performance, for both past changes and those to come, will be that patients have a better experience. “The patients are not having to wait as long. They’re happier. A happy patient takes you less time. This is a service industry. Satisfaction is what our product is.”