At a hospital in Pittsburgh, the emerging vision for the “hospital of the future” is described as giving the right patient, the right care, at the right time, in the right way, all the time.
If that sounds a lot like just-in-time production, there is no coincidence. In 2001, the University of Pittsburgh Medical Center Shadyside first applied principles of the Toyota Production System (TPS), the model for lean, on a few beds in a 40-bed surgical unit. Since the initial application on this “learning line” of 12 beds, Shadyside hospital has systematized the concepts into an approach called the Clinical Design Initiative (CDI).
Tami Merryman, vice president, Patient Care Services at Shadyside, describes CDI as a methodology to “redesign broken processes.” Key steps in the CDI approach, which emphasizes the plan, do, check, act (PDCA) cycle so central to TPS, are:
- Go to the scene where a problem occurs.
- Understand the current condition through direct observation of the problem.
- Determine the root cause by asking why five times.
- Redesign the process to eliminate the problem.
- Balance patient and staff satisfaction in designing solutions that are visual, simple, and unambiguous.
- Rapidly test the new process in a small area and make improvements.
- Identify and measure the desired clinical, satisfaction, and cost outcomes.
- Roll out the improved process to other areas.
On that first learning line, the CDI approach eliminated long-standing problems by exposing root causes. In the past, staff members developed work-arounds to problems that left root causes intact and created variations in how different people did the same work. “We gave people too many choices in doing work,” said Susan Christie Martin, director, Nursing Support Services. “We learned that it has to be either one way or the other. Stop giving people so many options and variations because it only causes confusion.”
Nothing was more confusing than the old routine for adjusting bedside pumps that dispensed pain-killing drugs intravenously to patients recovering from surgery. In what was assumed to be a necessary security procedure, only one set of keys for all the pumps was kept on the floor. The set was passed from nurse to nurse as needed during a shift. When a doctor told a nurse to change a patient’s drug dosage, she had to track down who had the set of keys for accessing the control unit on the pump. While the nurse roamed the floor looking for whomever had the key set last, the patient waited.
When CDI specialists closely observed the old process in action and asked why five times, the security procedure proved to be outdated:
1. Why do nurses have to hunt and search for keys to meet patient’s pain needs by adjusting epidural pumps?
They cannot make alterations in dosing without keys to access a pump’s keypad.
2. Why doesn’t the nurse have immediate access to the keys?
There is only one set of keys on the floor.
3. Why is there only one set of keys?
The key control procedure has been interpreted to mean that each unit can have only one set of keys per unit.
4. Why is the control requirement defined as one set of keys per unit?
The definition was based on historical practice. Before the installation of epidural pumps, pain-killing drugs were dispensed manually from a stock drawer, requiring that access be limited and closely controlled.
5. Is there a valid requirement for limiting the number of keys now?
No, only that we account for keys that are issued.
With input from staff, the CDI team created and tested a new process. Enough keys were made so every nurse who needed one on a shift had it. A supervisor assigned the numbered keys at the start of each shift, recording on a checklist who got what key. The supervisor kept unneeded keys locked in a drawer.
“At the end of a shift, I say, ‘Okay everyone give me your keys,’” said Tina Danzuso, a nursing supervisor. “In almost four years, we haven’t lost a key.”
Go See
To spread the use of the CDI methodology, the hospital taught administrators, supervisors, and nurses the fundamental technique of going to the scene to observe a problem. Much of the early training in the observation, PDCA, and flow techniques of CDI came from the Pittsburgh Regional Healthcare Initiative (PRHI), a coalition of regional hospitals, insurers, and businesses committed to improving healthcare. PRHI advisors included Haijme Ohba, head of the Toyota Supplier Support Center, Inc., and Harvard Business School Professor H. Kent Bowen and Assistant Professor Steven Spear, coauthors of “Decoding the DNA of the Toyota Production System” (Harvard Business Review, September-October 1999).
According to PRHI’s Debra Thompson, who delivered the initial training at Shadyside, applying lean principles to healthcare opens up “a whole new level of understanding and a whole new way of improving care to patients, making them safer, and making the work environment much healthier for our staff.”
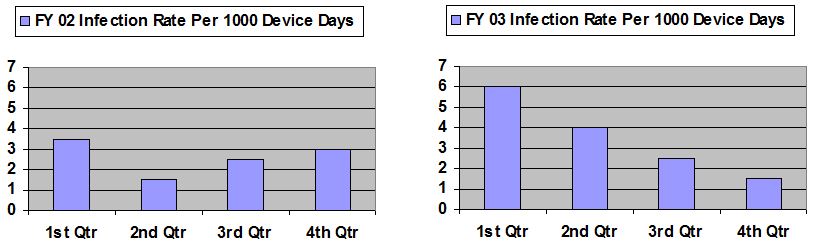
The training proved its value when a gradual increase in bloodstream infections was noticed in two units during late 2002 and early 2003. The infections were coming from intravenous catheters used to give patients medication or nutrition. (Such infections can be life threatening and cost an estimated $25,000 on average to treat at Shadyside.) Hospital guidelines called for a nurse to wear a cap, mask, sterile gown, and sterile gloves when changing a catheter dressing. The guidelines, based on recommendations from the federal Center for Disease Control, also covered how often to change dressings, what antiseptic to use, and how to clean the insertion point (swab back-and-forth, not in a circular motion).
Going to the scene of the problem, nurses made 13 observations of colleagues changing catheter dressings during a month. The observations found that some nurses neglected to wash their hands, used improper cleaning techniques, or had problems removing gloves from the special sterile kits provided for changing dressings. Nurses complained that gloves stuck together and ripped easily when being removed from the kit.
The hospital rewrote directions for inserting catheters and changing dressings to make them clearer so there would be fewer chances for confusion or individual interpretations. It educated staff about hand hygiene, proper cleaning techniques, and it switched to higher quality sterile gloves. Follow-up observations were done to make sure the new measures were working. By late 2003, the hospital had cut the infection rate dramatically and has sustained the lower fourth quarter rate in 2004. (A “device day” in the charts below is a day in which a patient had one or more catheters.)
Flow in Pathology
More recently, through a grant from the Jewish Healthcare Foundation, Shadyside used the CDI methodology to speed turnaround time in the Pathology Department, reducing the time needed to prepare and analyze some types of tissues samples from one or two days to the same day.
In many ways, the traditional layout and workflows of a Pathology Department resemble the traditional batch-and-queue organization of a factory. Equipment and activities are arranged by type rather than in the sequence needed to produce a product. Products (or tissue specimens) are processed in large batches then pushed ahead to the next process where they wait in a queue for the next steps.
The drawbacks of a batch-and-queue system include, among other disadvantages, long lead times as batches wait to be processed, delays in discovering quality problems hidden in the batches, unnecessary complexity in tracking and moving large lots, and high costs for the larger space, capacity, and manpower needed to process, store, and move large quantities. Such a system has no chance of achieving the short lead times, high quality, and low costs of a lean system that moves work smoothly and quickly in small batches or, ideally, in one-piece flow, from one process to the next.
Until its lean makeover, Shadyside’s Pathology Department operated in the traditional manner. Tissue samples arrived at the department from internal hospital units, such as surgery, or external doctors’ offices. The first stop was the gross room, so called because

it received large tissue specimens for sectioning into small pieces. Pathologist assistants cut the samples and dictated notes. They inserted the small pieces in plastic cassettes, roughly two-inches square. Batches of cassettes were loaded into the gross room’s two tissue-processing machines that replaced water in the samples with a liquid fixative during a 12-hour automated process that ran overnight.
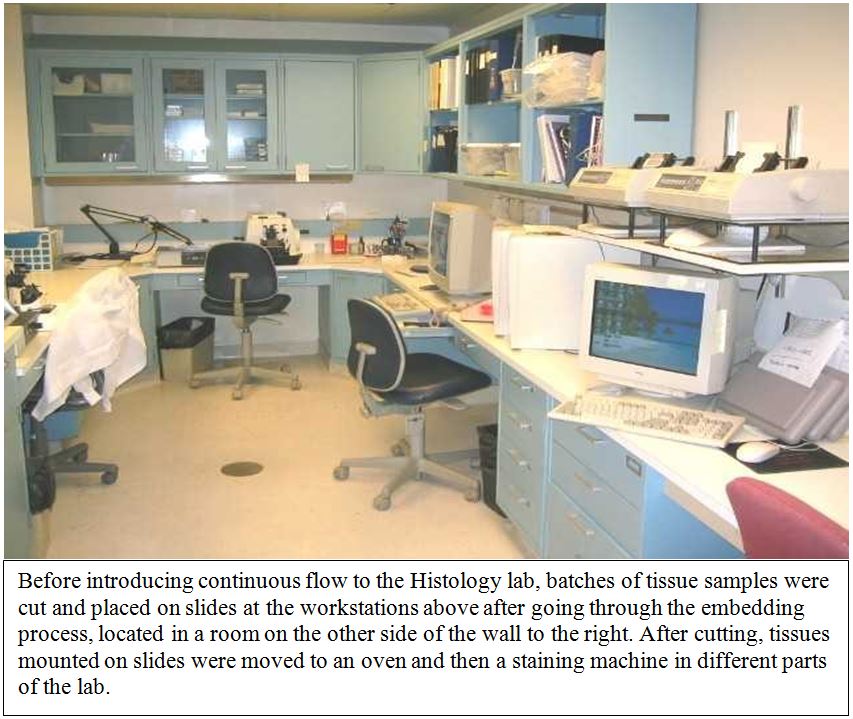
After fixing, histotechnologists moved batches of cassettes across the hall to Histology for embedding. At this step, the plastic cassettes were opened, the tissues were placed into metal molds, covered with a wax, and chilled for about 20 minutes until hardened. The wax made the tissues stiff enough to cut into paper-thin slices for mounting on glass slides. The histotechnologists identified samples by writing their unique identification numbers on all the slides.
Several technologists spent most of the morning embedding trays of tissue samples and labeling the accompanying batches of slides. In late morning, they moved the batches of tissues and slides from the embedding room through a doorway to an adjoining laboratory for cutting. “Everybody would come out from the embedding room at some point and begin using machines to cut the tissue and make the slides,” recalled Jennifer Condel, team leader, Anatomic Pathology.
At the cutting stations, technologists used tabletop machines called microtomes to cut samples into slivers and gingerly manipulate them with tweezers onto labeled slides. Then they loaded batches of slides, grouped by identification numbers, into racks and carried them to a small oven, located on a countertop in a different area of the lab. Seventeen minutes later, the wax had melted off, leaving only tissue on the slides. The slides were carried back to a machine near the embedding room for staining, an automated process taking about 45 minutes. In a final automated machine, the slides got a thin glass cover and a paper label. Then they went from the lab to a department transcriptionist, who matched paperwork and sent them to pathologists for analysis.
“Initially we had to understand the pathway” of how tissue moved through the department, said Condel. CDI specialists spent weeks observing the current state of how tissue came in and was processed. They envisioned an “ideal state” of continuous flow processing through the entire pathology value stream from gross room to pathologist. Since ideal states usually can’t be achieved immediately, the team identified intermediate improvement steps where it could begin to substitute continuous flow processing for batching.
Building Support for Change
Before making the improvements, Shadyside ran a workshop for department staff members that simulated how to apply lean concepts in an industrial environment. “It was a nice way to mimic a manufacturing setting and to get people thinking of how the concepts apply to their work,” said Condel.
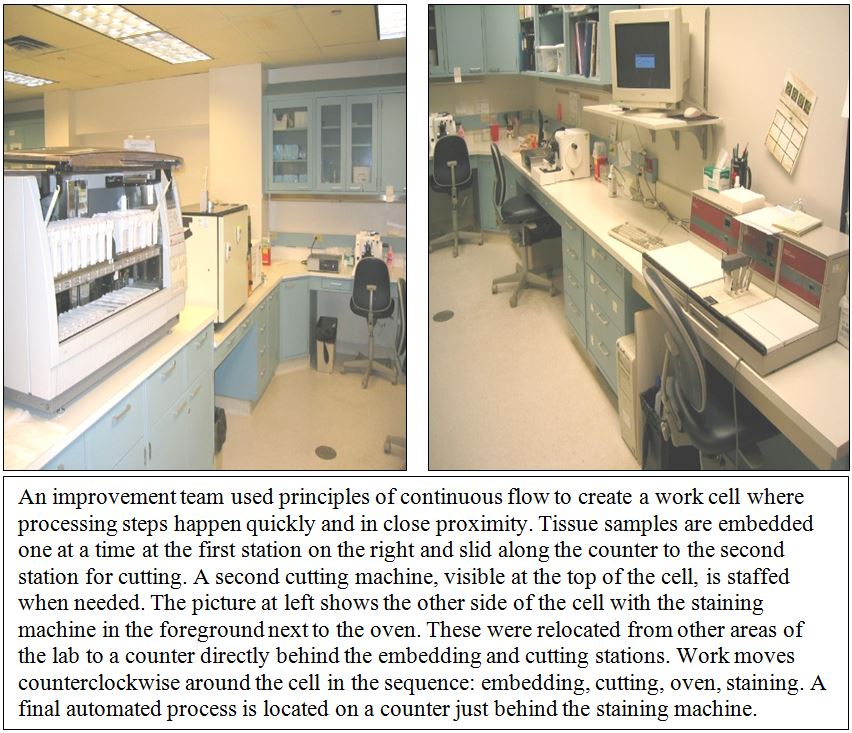
The workshop was followed by a 5S exercise to better organize the department and clear counter space so equipment could be rearranged into a cell containing embedding, cutting, heating, and staining in close proximity. CDI improvement specialists, department and PRHI staff, and hospital administrators, including Dr. Michael Becich, former Pathology Department chair, Dr. Stephen Raab, current Pathology chair, and David Sharbaugh, director, Quality Improvement and Information Analysis, stayed one night to reorganize the lab. Unneeded items were identified with red-tags and removed. Visual controls were used to arrange the remaining items in a neat and easy-to-use manner.
An immediate benefit was better inventory management. Even with a staff member spending eight hours each week checking inventory, which was stored in various locations, there had been over-stocking of some items and shortages of others. If someone failed to notice that an item, such as a chemical, was low, the department had to place expensive rush orders.
During the 5S house cleaning, staff members established dedicated storage areas, using labels and color-coding to identify the contents of each cupboard or drawer. Kanban cards with reordering information were attached to most items. When a reorder point is reached, the card is removed and hung on a board. Reordering now takes minutes a day. More important, the system virtually eliminated stock-outs and expensive rush orders while reducing inventory by 50% to 60%.
“It was rather exciting because many staff members were anxious to clean house but never had the opportunity,” said Condel. Enhancing the work environment helped to build staff support for the change process. The exercise also boosted management’s credibility. “We told the staff we were going to do it and we actually did it,” said Condel. “That had an impact by itself.”
The next step was to move away from batching and closer to continuous flow. The two tissue processing machines were moved across the hall from the gross room to a Histology room adjacent to the lab. Technologists were responsible for machine maintenance, so the relocation made upkeep easier. The gross room process of sectioning tissue samples remained in place because it required workstations with special ventilation and biohazard controls.
In analyzing workflow, the improvement team of staff members and CDI specialists questioned the 12-hours needed to prepare tissue samples for embedding. After study, the team decided that small pieces of certain types of tissues, such as skin, breast, or prostate biopsy samples, could be processed in three hours. As it happened, such samples also represented a fair portion of the daily workload. One of the two tissue processing machines could be used to run small tissue samples in three hours. The other machine would run samples needing 12 hours to set.
The team also questioned the batching that occurred between the embedding and cutting stations. “Why should the sample for patient one have to wait for patient 50’s sample to be done before I pass that work from embedding to cutting?” said Condel. An embedding machine was moved next to a cutting machine on a U-shaped countertop to improve workflow. Histotechnologist Mary Clancy, working with hospital carpenters, created small plastic containers that hold one tissue sample and all the blank slides needed. Instead of putting a dozen samples in a large plastic container for embedding, one sample at a time is embedded using the smaller containers. The technologist doing embedding slides a few small containers at a time along the countertop to the person alongside at the cutting machine. Because each small container holds one tissue sample and only its labeled slides, the chances of mixing up tissues and slides are greatly reduced. If a mix-up happens, it’s discovered quickly.
To complete the new cellular layout, the oven was placed on the countertop behind the cutter and the staining machine was moved behind the embedder. Each person operates two processes. If the workload is heavy, an additional person will work at another cutting station in the cell. The new arrangement allows tissue to move through the cell from embedding, to cutting, to the oven, to staining with fewer errors and in less time with few or no samples waiting between steps. Different tissue types require different quantities of slides, so the workload can be balanced by mixing in different types of tissue samples. Here is a summary of the improvements so far:
Pathology Department Improvement Box Score
| Turnaround | Small tissue samples are processed, sent to a pathologist for analysis, and the results returned the same day, instead of one or two days. |
| Quality | Mistakes are discovered immediately. |
| Inventory | Stock levels were reduced by to 50% to 60%; overstocking and rush orders due to stockouts were virtually eliminated. |
| Productivity | The lab is doing the same amount of work even though attrition and transfers have decreased staff by 28%. Time needed to order inventory was cut from eight hours weekly to minutes daily. |
The improvement team is continuing to refine the cell to get closer to the ideal state of continuous flow processing along the entire pathology value stream from gross room to pathologist. Still, the progress is affecting doctors and patients positively. Dr. Raab, the Pathology Department chair, said fellow physicians are adjusting to a steadier and more efficient workflow. When the department processed tissues in batches, pathologists spent much of the morning waiting for slides. “Now that slides come to them gradually in a flow method, they work continuously rather than having periods when they are working and times when they are not,” Raab explained.
Patients also benefit from the improved workflow. The reduction in turnaround time on small tissue samples means doctors get pathology results quicker. That means treatment or discharge from the hospital happens sooner. Since patients often are in the hospital awaiting diagnosis (many treatments occur on an out-patient basis), their hospital stays are shorter and hospital costs are less, Raab noted.
Managing Change
A group called the Core Team tracks the progress in Pathology and in other improvement projects. Shadyside also has used the CDI methodology to speed patient meal deliveries, eliminate wasted steps and paperwork from emergency room procedures, redesign nurses’ stations, improve the setup of operating rooms, and mistake-proof the distribution of medicine in oncology units, among other projects. Meeting weekly, the cross-functional Core Team of staff and administrators uses a grid to reviews the status of each project, plan next steps, and assign responsibility. The group’s nucleus includes Merryman, department directors and key managers, and improvement specialists. Other members come and go as needed, based on the projects underway.
“The grid lists all of our projects and the responsible people,” said Beth Kuzminsky, CDI improvement specialist. “We talk about each project and who’s responsible. We also discuss what are the next steps, who will be responsible, and who needs to help. Those are the people we invite to the next meeting.”
The CDI methodology for redesigning broken processes is paying off in one of the hospital’s biggest redesign efforts — changing the conventional way patients order meals during hospitalization into an educational process that teaches them how to chose foods that will optimize their health. The change is part of the national Transforming Care at the Bedside (TCAB) initiative, led by the nonprofit Institute for Healthcare Improvement (IHI) with a partial funding grant from The Robert Wood Johnson Foundation (RWJF).
Traditionally, hospital patients received pre-set menus for prescribed diets, such as low-salt or low-fat, based on their medical conditions. For patients, the prescribed menus did nothing to educate them about why certain foods were good choices and others weren’t. For the hospital, “the whole structure of the dietary department was built around distributing and collecting menus, collating menus, crossing out menu items, and making different types of meal trays,” said Merryman. “That’s gone. It’s all waste.” With their doctors’ okay, patients now order whatever they want from a standard menu, written and printed like the bill of fare at a good restaurant. Menu icons highlight good choices for certain conditions, such as recommended selections for patients who have diabetes, but patients are free to order what they want. Dieticians monitor patient selections. A trend in poor choices triggers an educational visit.
“If we see you eating poorly according to the medical diagnosis — for instance, if you are a cardiac patient ordering French fries everyday for lunch — then we’re going to send a dietician in to have a talk with you,” said Merryman.
Shadyside administrators expected food costs to increase with the introduction of the liberalized menu. Instead, costs dropped. In the unit testing the liberalized menu, food costs per tray fell from $1.37 to $1.15 in five months. Part of the reason was less paperwork for the dietary department. The other part was that patients “are more thoughtful” on the liberalized menu, according to Merryman. “The 80-year-old grandma who never ate more that soup and half a sandwich for dinner is not compelled to circle an item in each category on a restricted diet menu. She orders just what she wants.”
Doctors are happy with the new system, too. “Patients don’t complain about food,” Merryman said.
Shadyside is using some of the money saved to provide patients an evening snack. An aide walks around offering patients cookies and other snacks from a basket. “I believe spreading some joy in a very unjoyful environment helps healing,” she said.
At IHI, Vice President Pat Rutherford, who oversees TCAB, said Shadyside’s CDI methodology “was part of the reason they were chosen” for the national effort. “We saw that they were innovators and had numerous successful redesign efforts.” She noted that one of TCAB’s main themes is to improve the healthcare system’s efficiency through developing clinical processes that “are free of waste and promote continuous flow of information and value-added patient care.”
More broadly, TCAB is aimed at a comprehensive redesign of medical and surgical units within hospitals, and is addressing fundamental health quality issues: the need to reduce errors, customize care to patient’s needs and preferences, create effective care teams, enhance organizational efficiency, and maintain financial viability. The TCAB initiative was designed to draw on IHI’s experience in mobilizing teams of frontline clinicians and staff to make significant improvements in patient care, as well as its expertise in helping organizations provide the leadership and culture which embraces quality as its core strategy.. IHI and RWJF recruited three hospitals to test the viability of the TCAB approach through a rapid prototyping process. The hospitals, chosen in the fall of 2003 for their cultures of innovation and strong leadership, included: Seton Northwest Hospital in Austin, TX, part of the Ascension Health System; UPMC Shadyside, part of the University of Pittsburgh Medical Center (UPMC), and Kaiser Foundation Hospital in Roseville, CA, part of Kaiser Permanente.
Rutherford said IHI, based in Brookline, MA, is seeing a growing interest in applying lean concepts to healthcare processes. “There are a number of forward thinking hospital leaders who are looking at other industries for ideas that will help with the dilemmas and challenges facing the healthcare system, she said. “Shadyside was one of the forerunners in the country that began applying lean thinking principles to improve healthcare processes.”
“I’m very proud of the accomplishments we’ve made,” said Merryman, who knows there are always more broken process to find and fix to make the hospital of the future a reality. “We’ve just scratched the surface.”
For more information
University of Pittsburgh Medical Center (UPMC) Shadyside
UPMC Shadyside is a 486-bed advanced-care hospital that has been serving the residents of Pittsburgh and the surrounding area since 1866. UPMC Shadyside offers primary medical care, physician and nursing education, and a broad range of specialties that include cardiology, oncology, orthopedics, geriatrics, obstetrics and gynecology, vascular medicine, endocrinology, and more. Its medical staff includes more than 600 primary care physicians and specialists, many of whom have offices at the hospital and throughout the community. The University of Pittsburgh Medical Center is one of the largest nonprofit integrated healthcare systems in the U.S., consisting of 20 advanced care, specialty, and community hospitals and an array of other healthcare services.
Institute for Healthcare Improvement (IHI)
IHI is a nonprofit organization leading the worldwide improvement of healthcare. Founded in 1991 and based in Boston, MA, IHI is a catalyst for change, cultivating innovative concepts for improving patient care and implementing programs for putting those ideas into action. Thousands of healthcare providers, including many of the finest hospitals in the world, participate in IHI improvement projects.
Pittsburgh Regional Healthcare Initiative (PRHI)
Formed in 1997, PRHI is a consortium of 42 hospitals, hundreds of clinicians, four major insurers, dozens of major and small-business healthcare purchasers, civic leaders, and elected officials. It’s approach to healthcare improvement, is derived from the Toyota Production System (TPS).