The tools of lean are exciting to introduce and apply. At Washington Health System, we actually started our journey with a tools-based approach to lean (it doesn’t really work, but you knew that already…). We learned a valuable lesson through that approach – that as exciting as lean tools are, it’s important that creating the perfect tool doesn’t become your only focus. Often the phrase “I think it made things better” is a common answer regarding results; but now the question “What is the problem we’re trying to solve?” probably causes more frustration than anything else.
I remember one occasion when we were working on educating and coaching key team members and one of them said, “Your value stream map looks different than what I’ve seen in the past.” Since VSM wasn’t one of the tools that had been rolled out (attempting “Rapid Improvement Workshops” without VSM is an entirely different discussion), I figured this comment stemmed from some other previous experiences or self-study. Our conversation basically led us down the path of doing VSM the way I started in manufacturing, with the very standard symbols and using Visio to “make it look like a VSM.”
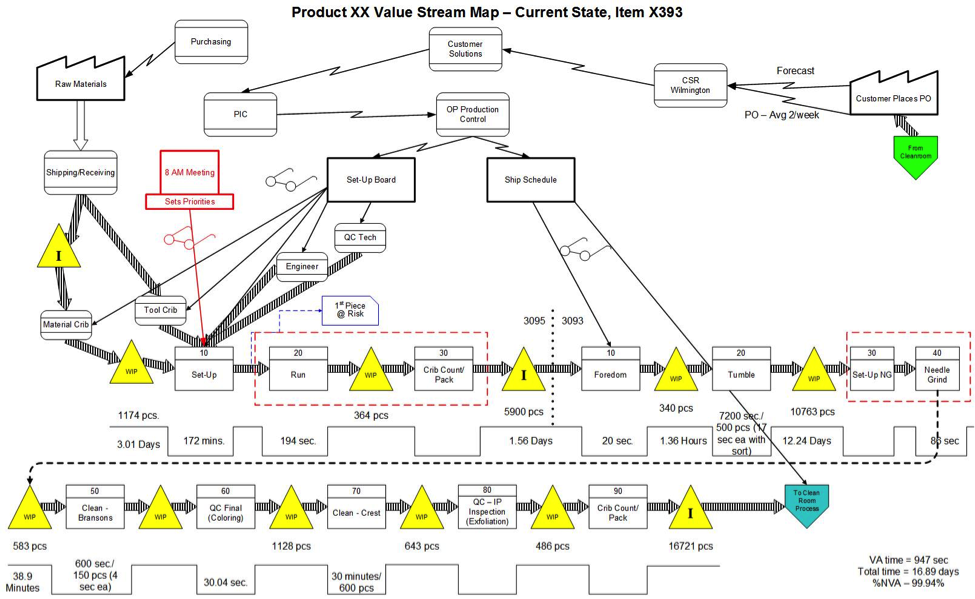
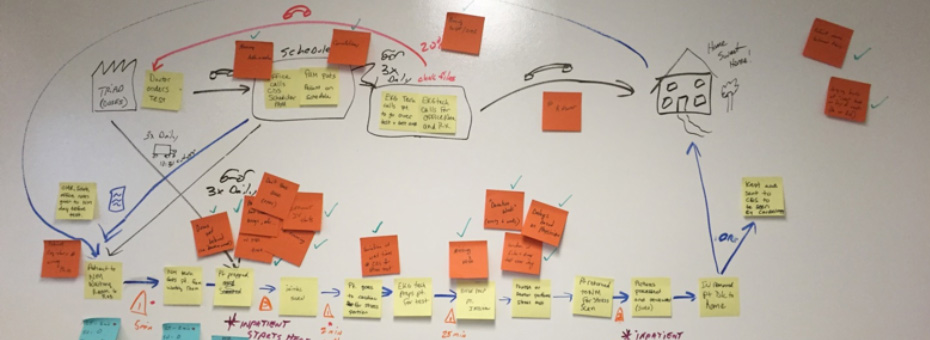
The event we were discussing was for a Nuclear Medicine clinical procedure, but it was focused primarily on the communication between the various functions as our patients went from being scheduled for the procedure at the doctor’s office, through registration, and then through the procedure. The key components we needed on that map were the process steps, the cycle time, the percent complete and accurate, the information flows, and the wait times. We used post-it notes on dry-erase to create our basic map.
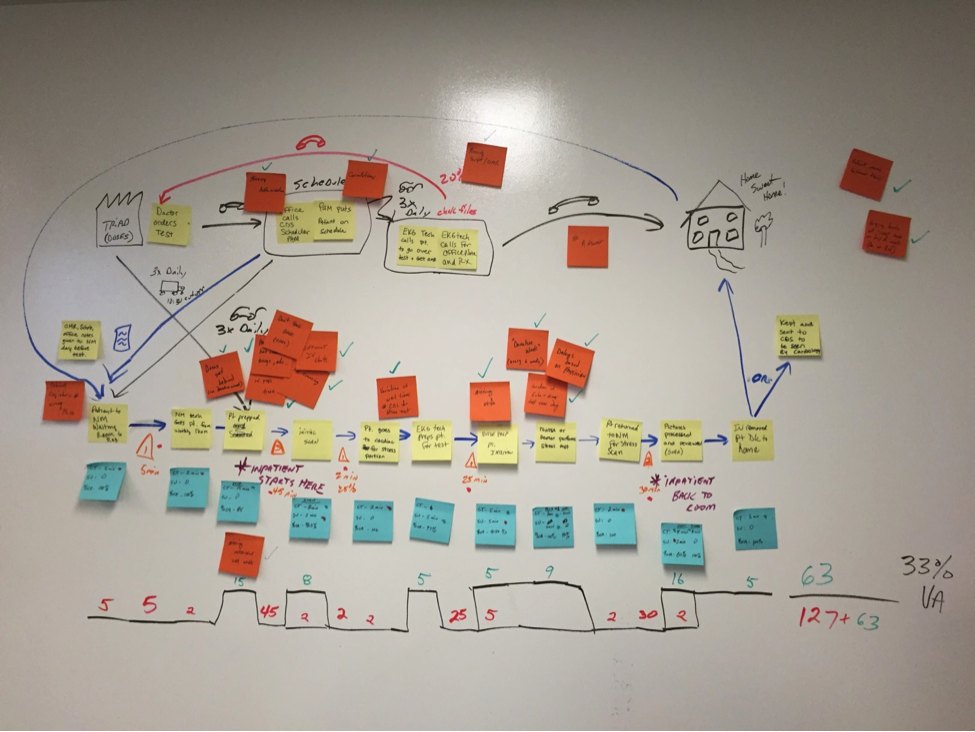
Then we focused on the opportunities, which led us to brainstorming, and onto creating an action plan to resolve the problems. So no, the VSM we created didn’t look exactly like one from Learning to See, but it did allow us to see what we needed to see. Our team was not going to change the clinical procedure, but we were able to reduce 90 percent of the “rework” that occurred in the scheduling process. We eliminated 75 percent of the support calls needed in Nuclear Medicine to correct information in the software system, 100 percent of the late starts in the morning which put the team (and patients) behind schedule all day long, and they eliminated 100 percent of the delays from patients that called the wrong number when returning calls due to using caller ID. We also found some patient comfort items which are hard to quantify, and weren’t needed to be quantified because they were just “the right thing to do.” Altogether, our relatively good patient satisfaction scores have risen higher.
What did we learn from all this? When embracing an improvement mindset, it is very important to understand the “why” of what you’re doing. What is the problem you’re trying to solve, and then, why are you choosing to use a certain tool? What is the result you hope to attain (while refraining from identifying the solution you hope to implement)? How do you envision the tools selected from the lean toolbox helping make the improvements? And if you think there’s a different way of applying a tool, ask, “Are we changing the tool to prevent us from changing the organization, or to better ensure change happens?”
What lean tools have you seen applied a little differently, and did it help move the organization forward? Or was it done out of convenience and comfort, resulting in little real change?